Globally, the COVID-19 pandemic has been an inflection point, bringing heightened awareness around the preparedness and resilience of public health systems in dealing with severe shocks. While the pandemic has accentuated the existing weakness in public health systems, for many, especially those belonging to marginalized sections of society, seeking healthcare has always been fraught with severe challenges and frictions.
This paper presents the findings from a two-year design research project conducted in South Africa and Bangladesh, which studied the challenges faced by health seekers, especially those whose ability to access healthcare is compromised by a range of vulnerabilities. These populations display remarkably adaptive behaviors and innovations that are aimed at mitigating the lacunae in public health systems.
In our analysis, these lacunae are articulated as points of friction, which are the gaps between the expectations of health seekers while accessing healthcare and the ability of health systems to meet these expectations. For vulnerable communities, these points of friction are often accentuated and more acutely felt. Taking a design thinking lens, we see these points of friction as opportunities for change that can potentially drive innovations in the public health space, leading to better health outcomes. The paper concludes with a set of design principles, which are meant to address the frictions identified during the course of the study and inform more user centered health systems in the future. Keywords: Health Systems, Human Centered Design, Design Research
INTRODUCTION
Health systems can be defined as a series of processes, actors, medical expertise and resources which work together to respond to threats to human health and well-being. One of the key outcomes of a strong health system is public trust in that system to look after the interests and needs of the public. People are willing to work with such health systems to protect the health of the broader society (Kittelsen & Keating, 2019). Weak health systems, on the other hand, are mistrusted by people and therefore have a diminished possibility of helping communities flourish and at scale interventions to being accepted (Ozawa & Sripad, 2013).
Designing for the Vulnerabilities of the Marginalized
Vulnerability is a concept that is often evoked in public health though many scholars have argued that its exact meaning is often vague. Vulnerability can loosely imply a particular status that may adversely impact upon well-being of individuals or groups (Wrigley & Dawson, 2016, p. 203). In our research, we chose to approach the notion of the vulnerability in an inclusive way and examples of vulnerable groups that we looked at range from large population segments such as low income groups and religious minorities to groups with specific disease burdens such as HIV or TB. Our research confirms the notion that vulnerability is an evolving status (Alwang, Siegel & Jorgensen, 2001), that even within populations that are inherently vulnerable for a range of reasons, there is a wide spectrum of cumulative vulnerability between individuals. For example, a poor family that has recently moved into a new neighborhood may be more vulnerable to a complicated and expensive health journey than a family that has deep social roots in the neighborhood and can leverage this social infrastructure to their benefit.
A core idea that emerged from study was that of a friction, which can be defined as the gap between the healthcare expectations of health seekers (referred to, at times, as seekers) and the ability and intention of the health system to meet these expectations. These frictions range from the lack of accessibility options for differently abled individuals to the real and perceived indifference towards crucial care networks1 that are likely to make a health journey successful. The frictions add layers of obstacles in accessing and receiving the care that health seekers need. We found that vulnerable populations face certain frictions that the general population may not and experience other frictions more acutely. As such, vulnerability to facing frictions while accessing care should be considered an important component of the cumulative vulnerability of an individual or a population group. Addressing these frictions or designing to mitigate them, while keeping in focus these vulnerable populations, will almost certainly address frictions faced by others who do not suffer (or at least not suffer to a degree) such vulnerabilities.
Understanding and Mapping Experiences of Health Seekers with Design Research
Globally, marginalized groups, such as the poor, religious minorities and differently abled are more vulnerable to health disruptions (Baah, Teitelman & Riegel, 2018) as well as frictions in healthcare access. Marginalization typically emerges from existing socio-economic and political realities. While design, which is an appropriate tool to address practical problems, can be leveraged to mitigate the effects of marginalization, it is incapable (without accompanying political and cultural processes) of eliminating marginalizations. One of the two core objectives2 of Amplifying Resilient Communities (referred to as project ARC or ARC) was to use the tools of design research including video ethnography to understand the experiences of health seekers as they interacted with a number of healthcare options. Our primary focus was public healthcare but we also studied private healthcare including traditional and non-medical care, as most health-seekers we studied lived within pluralistic healthcare ecosystems. By documenting and analyzing these health journeys, we were able to identify and categorize a number of frictions that people experience. For seekers, these barriers can lead to a number of negative consequences such as an inability to identify the right avenue of care and engage with the treatment process. For health systems, these frictions are barriers in achieving public health goals such as identifying the right treatment plans for people, ability to reach vulnerable populations, responsiveness/resilience to shocks, among others.
COVID-19 as the Inflection Point
COVID-19 created a volatile situation for health systems and seekers. Interactions with health systems, which were already riddled with frictions for seekers, were more strained. Due to physical distancing measures, government shutdowns and other transmission reduction measures, as well as the widespread commandeering of medical facilities for COVID-19 testing and treatment, people missed essential health services such as antenatal care, vaccines, HIV testing and medication, tuberculosis care, and catastrophic health event access3. Alongside this, the stress put on frontline health workers and resources was unprecedented. Project ARC sought to gain a deeper understanding of how vulnerable populations4 interact with healthcare systems (institutions, facilities, and providers) during and after COVID-19 by centering their voices, stories, and experiences. Using COVID-19 as an inflection point, we aimed to understand where the weaknesses were in health systems especially under stress.
Informing the Design of Future Health Systems Interventions
Another core objective of ARC was to frame a set of design principles that are aimed at addressing the frictions that were identified. These principles reflect the lived and felt needs of people — some of the most vulnerable users in stretched health systems. These are aimed at service and product design in health, which could be optimized to enhance maximum uptake, through a deep understanding of the seekers and the context of their lives. In ARC we could make suggestions for building back health systems, something that many stakeholders in global health imagined as an appropriate response to the failures experienced during Covid. But as discussed above, ARC, a design led inquiry was not positioned to make the changes to health systems; design principles, therefore became a way of interjecting important human-centered considerations into the conversation.
Project ARC Team
Project ARC, is an interdisciplinary consortium consisting of: Ipsos, a global insights company composed of global health experts, anthropologists, and psychologists; Matchboxology and Quicksand, long established human centered design companies based in South Africa and India respectively; independent consultant Anabel Gomez who brings an implementation perspective to solutions for key public health challenges. Quicksand worked closely with partner James P Grant School of Public health (JPGSPH) of BRAC University, who led field activities in Bangladesh. JPGSPH took the lead in recruitment and field research, while Quicksand led research design, training for the field researchers and analysis & synthesis. Project ARC was also supported by local champions networks (LCN) in both South Africa and Bangladesh. Additionally, we also consulted a global advisory group towards the latter stages of the study5.
METHODOLOGY: DATA COLLECTION
Project ARC conducted primary research in two phases in both South Africa and Bangladesh. While each phase included design-led qualitative approaches, the first phase (Round A) intended to build a foundational understanding of health seeking practices, social relations of influence and trust within communities, the spaces that people seek care at, and the impact of COVID-19 on health seeking behaviors, perceptions, and health provision. Round B was then designed to build upon the learnings from round A, fill gaps in our research, and most importantly, dive deeper into the life histories and care journeys of health seekers — with the aim of arriving at key friction points, and opportunities of change within health systems. Figure 1 below presents the broad flow of the key milestones of Project ARC.
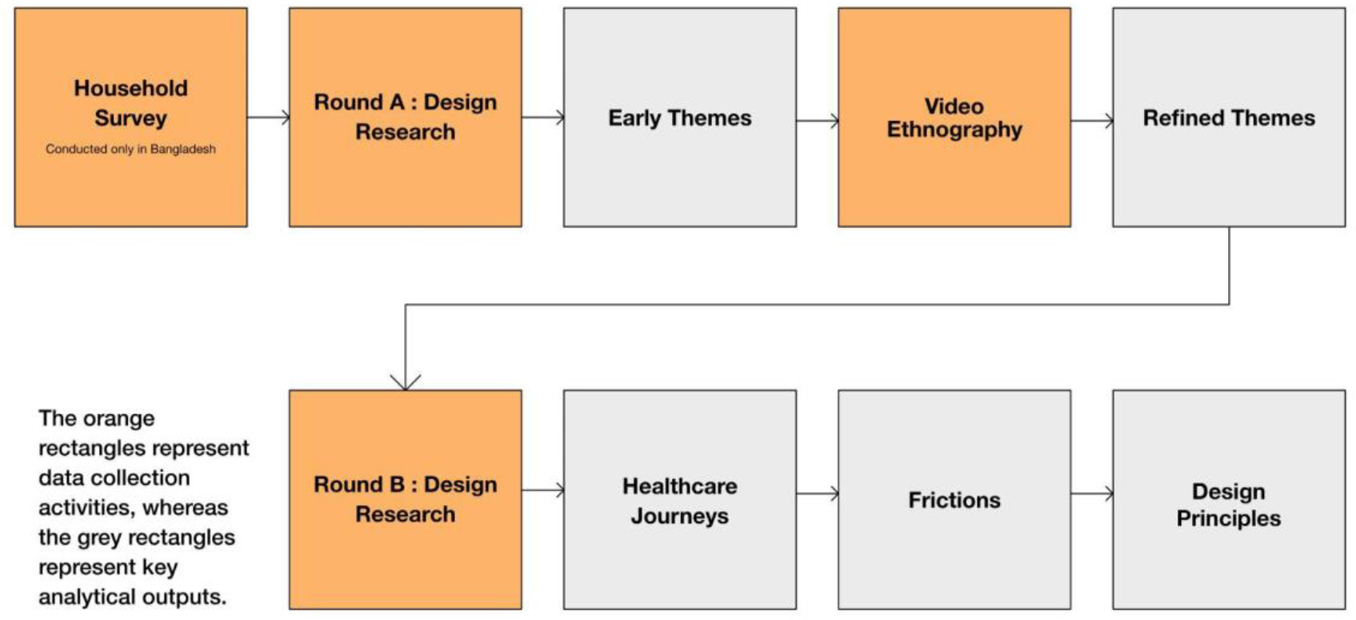
Figure 1. ARC methodology outline. Flowchart © Project ARC.
Household Survey
A household survey was conducted in January 2021 with 619 individuals across 595 households in Dhaka (Korail urban slum), Bogura (rural) and Narayanganj (peri-urban). The primary objectives of the household survey were twofold. Firstly, to get a broad and early sense of the factors that respondents were concerned with when it came to health and health access and secondly to recruit the participants for the subsequent phases of research.
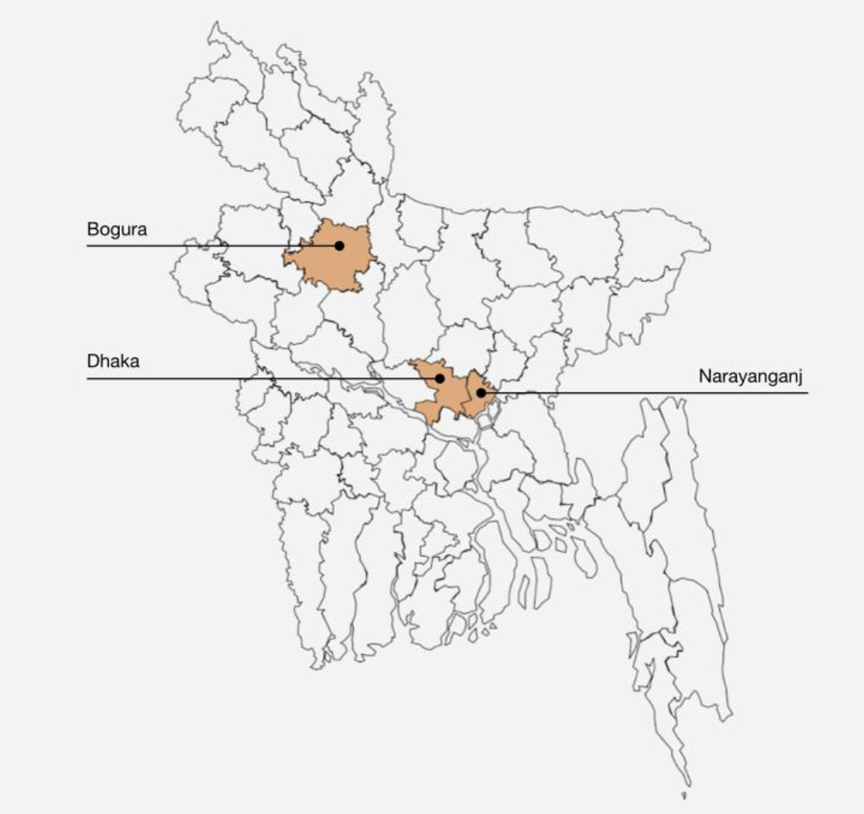
Figure 2. Research locations in Bangladesh. Illustration © Project ARC.
Round A: Design Research
Design research was conducted across South Africa and Bangladesh between February and March 2021. In South Africa we recruited respondents using an external local organization (Brand iD) and through the Center for HIV-AIDS Prevention Studies (CHAPS) clinics using purposive sampling with guidance and assistance from the Matchboxology team. Screening criteria included: 18-49 year olds living in one of the following four provinces — Gauteng, KwaZulu-Natal, Mpumalanga, and Western Cape. An even split of women and men were recruited from among: patients, providers, and community leaders (self-identified). Eligible healthcare providers (HCP) included: community health workers (CHWS), receptionists, nurses, laboratory staff, administrators, managers or physicians. 85 individual in-depth interviews were completed in total, with 69 patients or “health seekers”, 28 health care workers, 30 community leaders, 42 wildcards6, 11 non-health seekers and 5 “other” respondents.
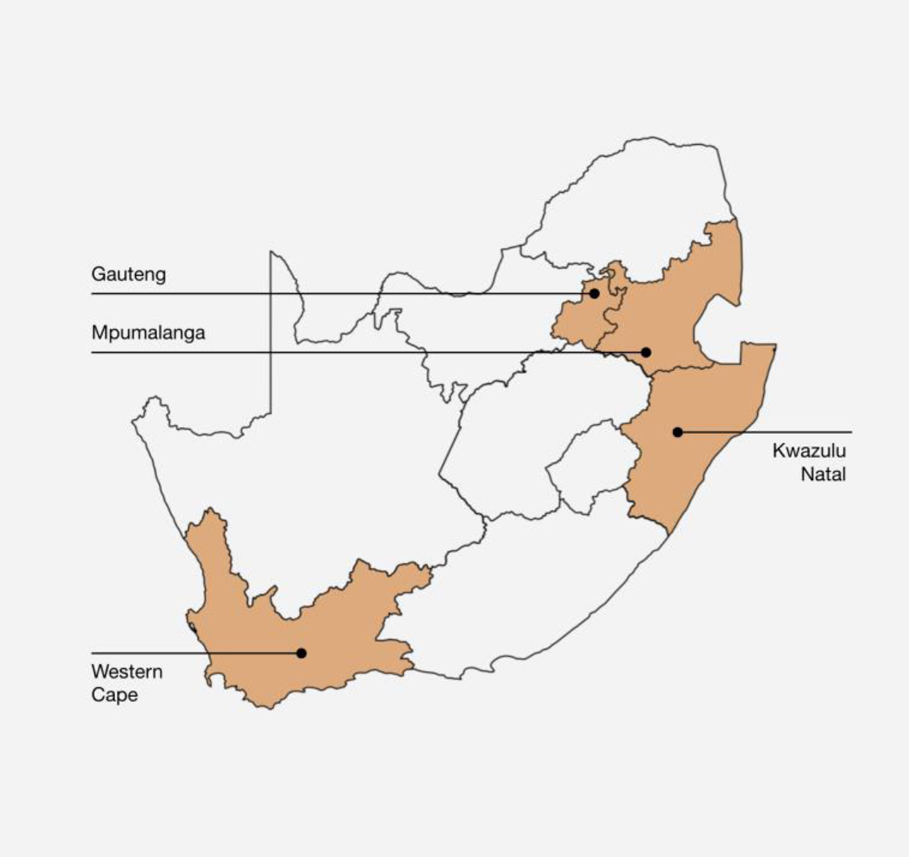
Figure 3. Research locations in South Africa. Illustration © Project ARC.
In Bangladesh, where the household survey was conducted, respondents were selected from among the survey participants. We were particularly interested in including individuals who represented disease burdens that health systems in Bangladesh have prioritized (including TB, Diabetes, Hypertension, COVID-19 etc). Furthermore, we ensured diversity in terms of gender, age, ethnicity and of-course geography. We also purposively sampled for differently abled individuals and religious minorities. A total of 156 participants participated in Round A in Bangladesh across 40 health-seeker in-depth interviews, 33 provider in-depth interviews, 6 health seeker focus groups, and 10 health provider focus groups.
Interviews and focus group discussions were based on qualitative immersion guides that demonstrated Human Centered Design approaches. This allowed the interviewers to also explore areas of interest that arose during interviews, which were not in the original guide. During research planning, global immersion guides were first created with the overall lines of inquiry. Subsequently, localized guides were created to ensure sensitivity to local contexts (including language localization) through detailed discussions with field research partners. Additional design research probes accompanied the immersion guides to support the research inquiry. In design research, probes allow researchers to engage participants beyond answering questions and invite them to participate in collaborative discovery by mapping and reflecting on their life experiences (Mattelmäki, 2006). Figures 4.1 and 4.2 below show one of the research probes we used to collaboratively map key influencers in an individual’s information ecosystem.
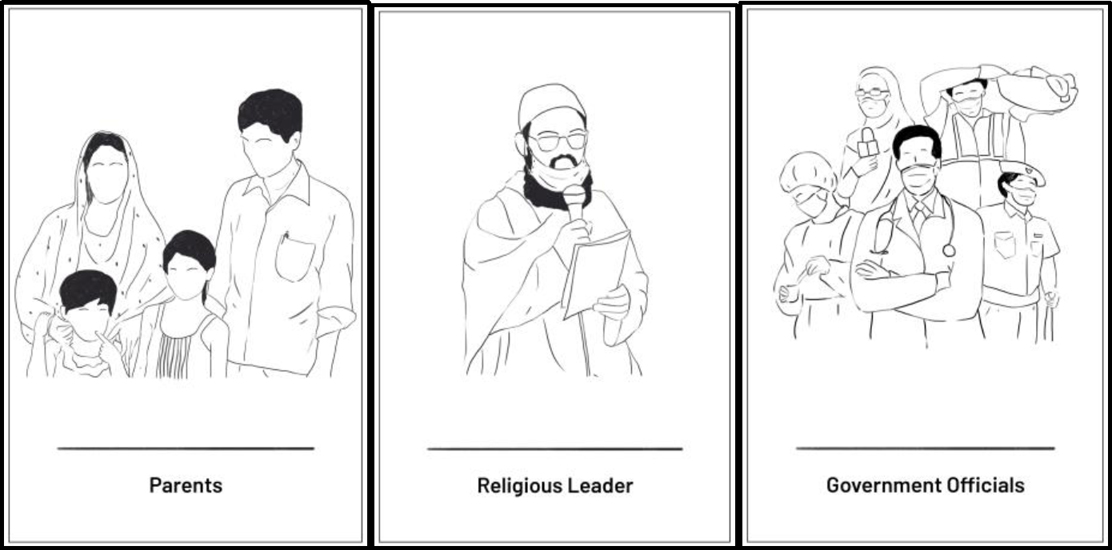
Figure 4.1. Research Probe: illustrations of a few influencer cards — parents, religious leaders, and government officials — from Bangladesh used to dive deeper into questions of trust and access in the information space. Illustration © Project ARC.
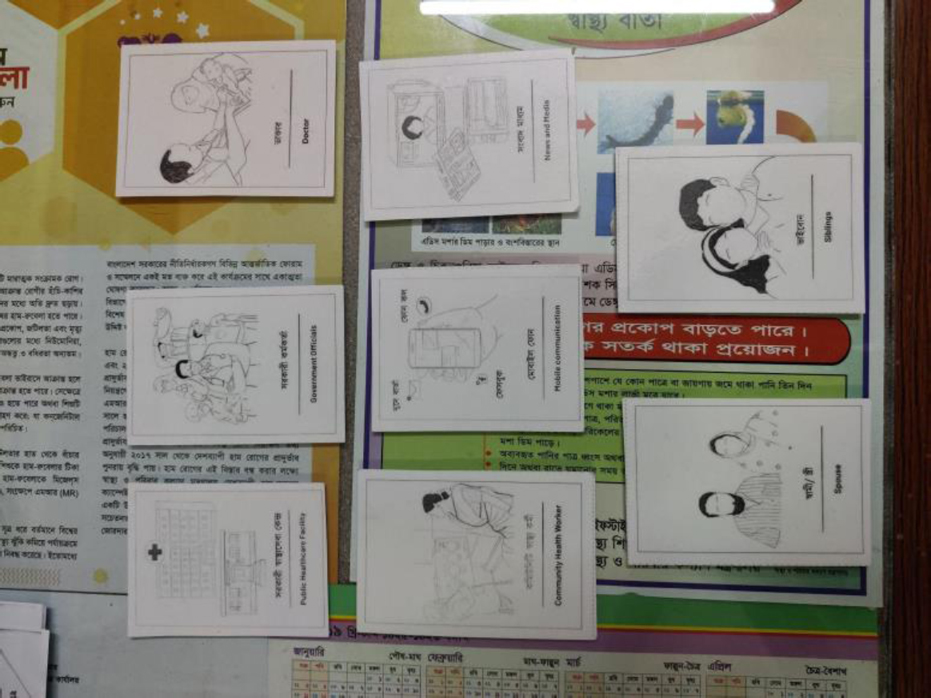
Figure 4.2. Influencer cards laid out during the research activity at a respondent’s home. Photograph © Project ARC.
Since Round A was conducted as the first COVID-19 wave was still fresh in the memories of participants, a significant part of the inquiry focused on understanding healthcare experiences during the peak of the pandemic, especially during lockdowns. Apart from this, our inquiry focused on these broad areas:
- Deepening our understanding of what “health” and “healthcare” mean for our participants.
- Deepening our understanding of how and where participants sought care, including non-formal avenues such as traditional healing.
- Collecting the outlines of a number of participant health seeking journeys either during the pandemic or before it.
- Understanding the influencer ecosystem around individuals, which shapes their perception of their own health and public health initiatives and directives.
Considering that further rounds of research (including video ethnography and the second round of design research) were to follow this phase, the lines of inquiry were deliberately kept broad so as to elicit a wide range of responses, which could inform further rounds.
Video Ethnography
Filmed ethnographic research was conducted to a) lend complexity and depth to the research overall, as well as provide valuable socio-cultural context to support the design phases of Project ARC and future dissemination and b) build on the findings and emerging themes from Round A, using a participant led approach.
In South Africa, a week-long digital ethnography was conducted with 20 participants recruited from the round A in-depth interviews. The research was intended to be participant led and iterative in approach. Whilst a guide was created in response to the themes developed from Round A, participants were encouraged to take an active role in directing the research and film what was most interesting to them when it came to interactions with the healthcare system.
Out of the 20 participants in this portion of the study, five participants each were based in one of the four South African provinces. All participants were health seekers with varying health burdens, from TB to maternal and child health. Furthermore, two to three participants were also community leaders, and one was a traditional healer. None were health workers, except those who are engaged in non-allopathic health systems.
Each participant had a 1-hour long interview with their ethnographer to go over the objectives of the project, their participation and consent, training on self-filming, and to dig deeper into their interactions and existing relationships with the health system. These tasks were intended to provide an understanding of the participant’s home life, cultural and social context, their networks, as well as their relationship and understanding of health, and the healthcare system. The tasks involved asking the participant to film: their daily routines, family interactions, community events of occasions, and interactions with the healthcare system and reflections on their experience of this e.g., queuing up to see a doctor or visiting a pharmacist etc.
In Bangladesh, due to constraints on travel during the pandemic, participants were recruited as ‘ethnographers’ of their own communities. This meant that this phase of research was in part guided by what our participants saw as most interesting and important when it came to their interactions with the health system, and their cultural context more broadly.
A total of 8 local informants led the ethnography: in Dhaka, 1 senior staff nurse from a non-governmental organization and 1 midwife; in Narayanganj, 2 students with smartphones who were respondents from Round A and 2 volunteer health workers; in Bogura, 1 respondent from Round A with a smartphone and 1 contact of a BRAC field organizer.
A local Bangladeshi ethnographer, together with the Ipsos team, was responsible for interviewing the informants, coordinating, and providing instructions as to what to film and what questions to consider and respond to. The ethnographic research began with an hour long interview with the intention of uncovering and understanding the informant’s interactions and existing relationship with the healthcare system, going over the objectives of the project, their participation and consent, and training on self-filming, as well as filming others and collecting consent.
These initial ‘tasks’ involved filming: daily routines, household dynamics, religious rituals and events, as well as responding to questions around notions of health and health care to ascertain how informants as well as their communities understood and defined health. After each task was sent in, the local ethnographer responded with probing questions, and a conversation between the ethnographer and the informant would lead to further learnings. After completing the first four tasks, the informant discussed potential further lines of inquiry, based on what was found during design research in Round A, with the local ethnographer and Ipsos team. The informant was allowed to lead this phase, with the intention of probing deeper into their own networks, and into themes and questions raised in the first round.
The findings from video ethnography helped shape Round B lines of inquiry, including a focus on: the role of pharmacists in the healthcare system, aspects of healthcare journeys outside of the encounter between providers and patients (considering the impact of the experience of the queue for example), and the role of family members and community influencers when it came to understandings of health and relationships to the health system.
Round B: Design Research
The second round of design research was conducted across South Africa and Bangladesh between September and October 2021. In South Africa analysis from the ethnographic inquiry showed gaps in understanding contraceptive disruptions and birth experiences, as well as a need to better understand health journeys. Therefore, this was the focus for Round B, as well as CHWs and pharmacists in their role as HCPs. Participants included: 24 women of reproductive age (WRA) selected from Round A, with whom group sessions were conducted based on contraception history and life cycle along with 7 in-depth observational studies, 3 CHWs, 3 pharmacists, 3 clinic administrators and 7 local social innovators working in health provision. The women were interviewed in groups of 3-4 in both KZN and Gauteng. Pharmacists, hospital administration and CHWs were recruited with the assistance of CHAPS. Social innovators were also interviewed in this round. Innovations were identified through gray and academic literature reviews conducted by the Matchboxology team.
In Bangladesh, analysis from the video ethnography revealed no particular gaps and the design research retained focus primarily on health seekers, with some sessions and activities with HCPs. The recruitment strategy for this phase of the research consisted of revisiting participants from Round A as well as recruiting new participants, both seekers and providers, through the networks of JPGSPH. A total of 72 participants participated in Round B in Bangladesh : 26 in-depth interviews with health seekers, 11 interviews with influencers, 13 interviews with health care providers, 6 interviews with community leaders, 13 facility observations, 8 shadowing sessions with CHWs, and 6 focus group discussions with community health workers. Interviews with social innovators were also conducted. These were identified by the JPGSPH team as well as through gray and academic literature reviews conducted by the Quicksand and JPGSPH teams.
Across both countries, Round B was intended as a more focused and detailed inquiry around early themes already identified and prioritized in Round A and ethnography. As such, a smaller number of participants were selected for this round and the interviews were significantly longer. As in Round A, our inquiry in Round B also included the use of design probes. One of the tools we used extensively was a healthcare journey mapping tool. This was a critical part of our inquiry as we wanted to capture detailed health seeking journeys in this round.
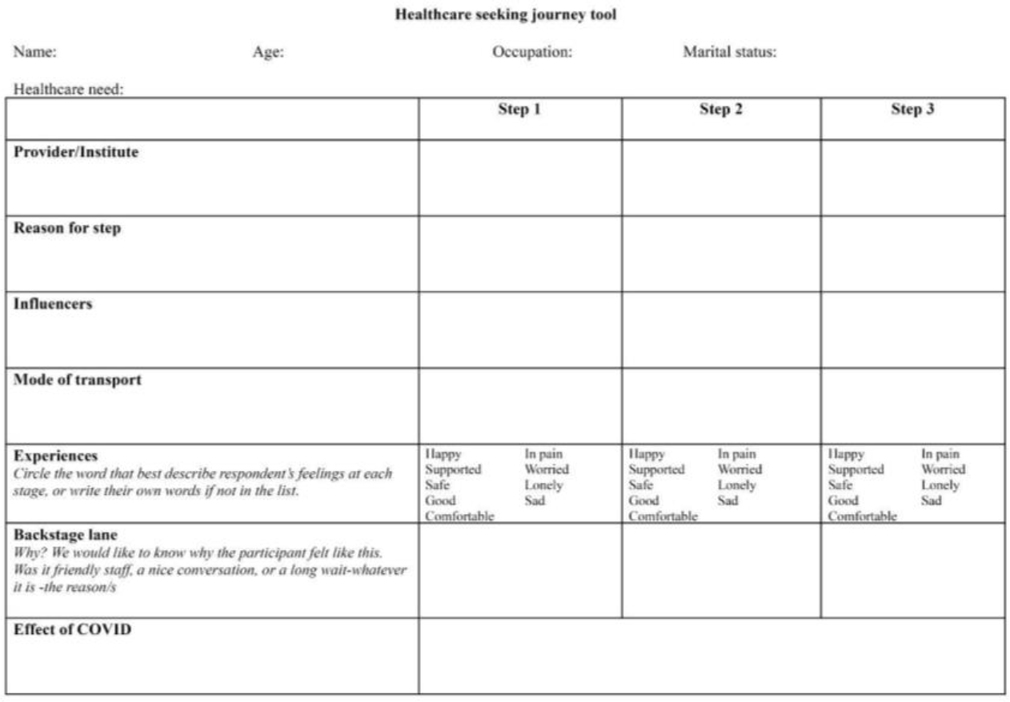
Figure 5. A tabulated version of our journey mapping tool. Tool © Project ARC.
Another probe we used was a set of illustrated scenarios, which were inspired from the learnings in Round A. The researchers would show these to participants and ask for their observations and reflections. Scenarios helped research participants engage with complex and sensitive topics by empathizing with the character in the narrative as someone like them, rather than responding with their own experiences alone to the researcher, which could be hard for them to recall, talk about, reflect upon, and critically examine. They also helped in concretizing (Carroll, 2000) abstract concepts in people’s experiences, whether they were motivations, fears, aspirations, problems etc. This led to rich discussions with the participants.
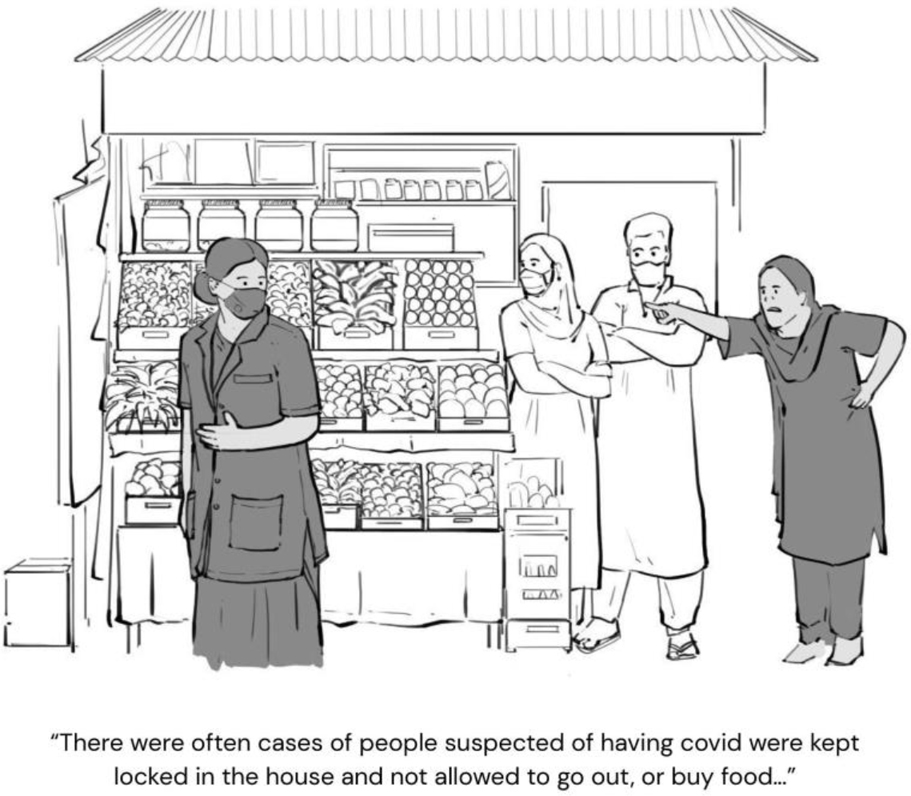
Figure 6. One of the scenarios that our participants were asked to reflect upon. Illustration © Project ARC.
Apart from detailed individual interviews with seekers and healthcare providers and focused group discussions with providers, Round B also included a couple of observation techniques including fly on the wall observation (Gkatzidou, Giacomin & Skrypchuk, 2021), which researchers used to observe the goings on in healthcare facilities and pharmacies and shadowing (Hamada, 2019), which researchers used primarily to follow CHW to better understand and document elements of their care-provision within the communities they operated in.
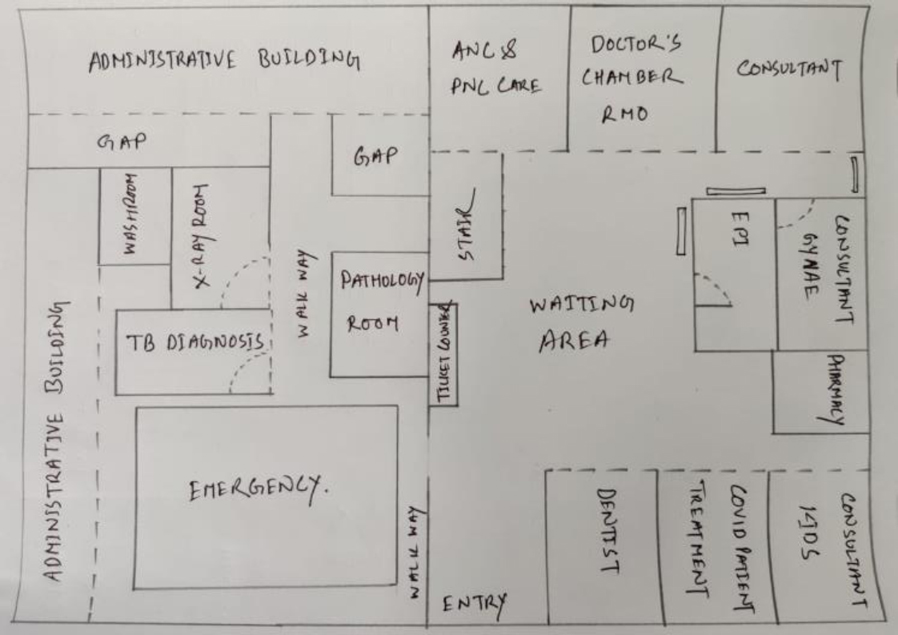
Figure 7. An observation map of a Upazila Health Complex in Bogura created by one of the researchers. Illustration © Project ARC.
Research Activities and Data Collection: Global Project ARC Research Team
Virtual workshops were conducted over Zoom in November and December 2021 to align on key themes identified in the interviews from Rounds A and B of the research in South Africa and Bangladesh. An in-person workshop was held in London in May 2022 to generate ideas based on insights and analysis from all rounds of research.
METHODOLOGY: ANALYSIS AND SYNTHESIS
The analysis was driven largely by a bottom up design thinking approach coupled with video ethnography analysis. The diagram below represents the process of building from early community observations to Design Principles, which were our final outputs. This was a highly bespoke analysis and synthesis process that was evolved by a multidisciplinary team, who were able to bring to bear best practices from a number of research and analysis traditions7. Ultimately it was a process rooted in design thinking, which by its nature is able to accommodate a multitude of approaches by understanding and leveraging their complementary aspects (Andrawes, Johnson & Coleman, 2021).
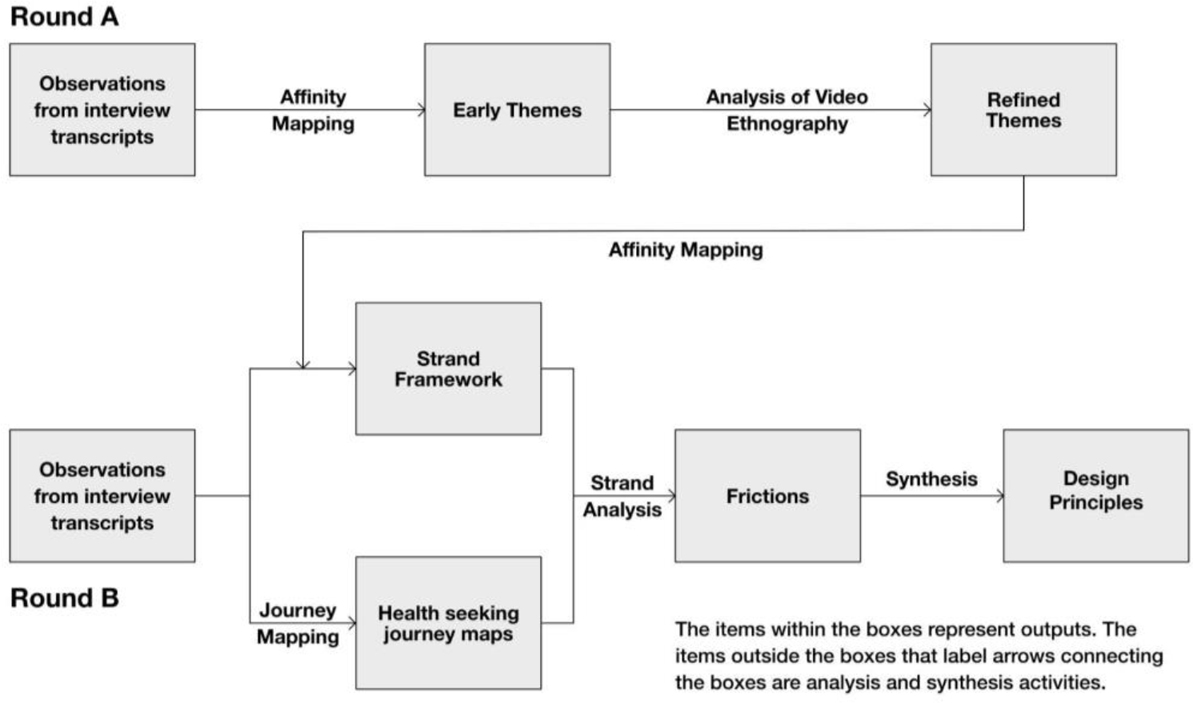
Figure 8. Process map of analysis and synthesis activities. Flowchart © Project ARC.
This section focuses primarily on analysis and synthesis along with descriptions of some interim outputs where needed. The main outputs, i.e. the Frictions and Design Principles are discussed in the outputs section.
Round A: Mapping Affinities to Arrive at Early Themes
Takashi Iba et al describe clustering as a pattern mining activity (Iba, Yoshikawa, & Munakata, 2017). Clustering as understood in the context of Project ARC can be understood simply as the act of bringing together observations according to some set of rules. In the beginning of this activity the patterns are not clear. At this stage, the process is driven by trial and error. As more and more observations are brought together, however, a pattern or more likely a number of patterns, which themselves are likely linked, emerge. Clusters begin to represent meaningful themes, the linked themes themselves evolve into narratives and at times, insights into the phenomenon being researched.
Affinity mapping, as the process of clustering is usually referred to in design thinking, formed the core of our analytical process. Research teams across South Africa and Bangladesh conducted their analysis together. This took the form of a digital whiteboard (we used the MIRO platform) where findings from research interviews were clustered together highlighting themes that emerged across both countries. While we did find a lot of resonance across the two countries, there were some themes that were more prominent in one rather than the other. Briefly, the themes identified in the first round of research included:
- Dialogues as Pathways to Action, which explored the criticality of dialogue between health seekers and the health system.
- Contextualisation of information, which focused on the need to make health messaging and information relatable to health seekers.
- The trust ladder, which broadly explored the crucial role of trust in the public health ecosystem.
- Limited access for the poor, which focused on the incredible challenges that those in the lower socio-economic segments face while seeking healthcare
- Pandemic related disruptions
- Social Health Infrastructure, which looked at care networks around individuals and the crucial role these networks play in keeping individuals healthy and in helping health seekers access healthcare.
- Healing and treatment, which looked at the idea of healing when compared to medical treatment and the role that this idea plays in shaping perceptions among seekers around modern medicine.
- Income vs Healthcare Expenditure, which focused on understanding healthcare expenditure within the context of the overall income of a household.
- Fear and behavior, which, especially in the light of the pandemic, looked at how fear shapes behavior of health seekers.
- Loneliness and disconnection, which focused on the way the pandemic had isolated health seekers and the impact that this was having on their mental health.
Refining Themes: Ethnographic Analysis
The data collected as part of the video ethnography was analyzed separately. To analyze ethnographic data, video clips were first uploaded to video management platform Big Sofa and translated. Multi-day analysis was then conducted online using an analytic framework that contained pre-determined questions to be answered/explored by each ethnographic task.
In South Africa, the local ethnographer, together with the Ipsos team, analyzed the footage and responses using an anthropological lens. Of particular note during this phase was participants’ experiences queuing up to access public healthcare, the experience in the queue itself, contrasted with other experiences of healthcare such as visiting the pharmacy, using traditional medicine etc. Further tasks probing deeper into healthcare experiences were discussed between local ethnographers and the Ipsos team, and were proposed to participants. This was to ensure the right questions were being asked and that the research was participant led.
After these final tasks were complete, the Ipsos team and local ethnographers collaboratively analyzed the new footage, responses from participants, and fieldnotes from interviews with the participants (conducted throughout the research process). Particular attention was paid to the cultural context of the participants, their family and community dynamics, as well as the relations between various actors within the healthcare system.
In Bangladesh, after the ethnographic phase was complete, the video footage as well as field notes from the interviews, and observations from the local ethnographer, were analyzed. Three internal analysis sessions took place, whereby an anthropological lens was applied to the findings with the intention of understanding how cultural context shapes and may determine understandings of health and relationships with healthcare systems.
Analysis Frameworks: Strand Framework and Mapping Journeys of Health Seekers
An affinity mapping or clustering approach was used for analyzing the data collected from the second round of design research as well. However, in this round, since refined themes had already been articulated, there were pre existing clusters to serve as starting points for the exercise. Two clear pathways emerged from this analysis, which led to the identification of Frictions and Design Principles, the core outputs of Project ARC.
Strand Framework
Over the past 15–20 years there has been widespread acceptance of the social determinants of health (Braveman, Egerter, & Williams, 2011). The World Health Organization (WHO) recognises a number of factors that can influence health in positive and negative ways (Social determinants of health, n.d.). These are:
- Income and social protection
- Education
- Unemployment and job insecurity
- Working life conditions
- Food insecurity
- Housing, basic amenities and the environment
- Early childhood development
- Social inclusion and non-discrimination
- Structural conflict
- Access to affordable health services of decent quality
To complement and build on these determinants, which are ostensibly conditions that influence the health of individuals as evidenced by over a decade of research, the Project ARC team sought to discover and develop the factors that health seekers themselves identify as constituent parts of their health. Our core line of inquiry here was, “what does health mean for individuals and communities”. Unsurprisingly the constituent parts of health we discovered are related to the social determinants of health, but unlike the social determinants of health, which are (or at least understood as) factors that influence health, the strands we discovered were, in many ways, for seekers, health itself. One of the key insights that emerged in ARC was that health seekers understand their own health in an expansive way. This understanding of health can be broken into constituent parts for analytical purposes but for health seekers, they are not discrete components that they consider individually but are more akin to an indivisible whole of entangled concerns that drive their perception of health. For Project ARC, this led to the Strand Approach of understanding health. The strands that we identified were:
- Physical health – the ability to perform the daily activities of one’s choice in the absence of illness.
- Emotional Health – the psychological and emotional wellbeing of an individual.
- Financial Health – the ability of a person or household to support and look after themselves.
- Social Health – the ability to create healthy and positive interpersonal relationships with one another to foster a supportive community.
- Spiritual Health – the feeling that an individual is living a meaningful life, in line with their moral code of conduct and belief system.
- Environmental Health – the ability to live in a safe, stable environment in which an individual can live their life the way that they choose to.
According to our findings these six strands come together to form a holistic perception of health among individuals and communities and stress on any of these strands is often seen as a stress on their overall health. The diagram below visualizes this approach as a rope consisting of strands.
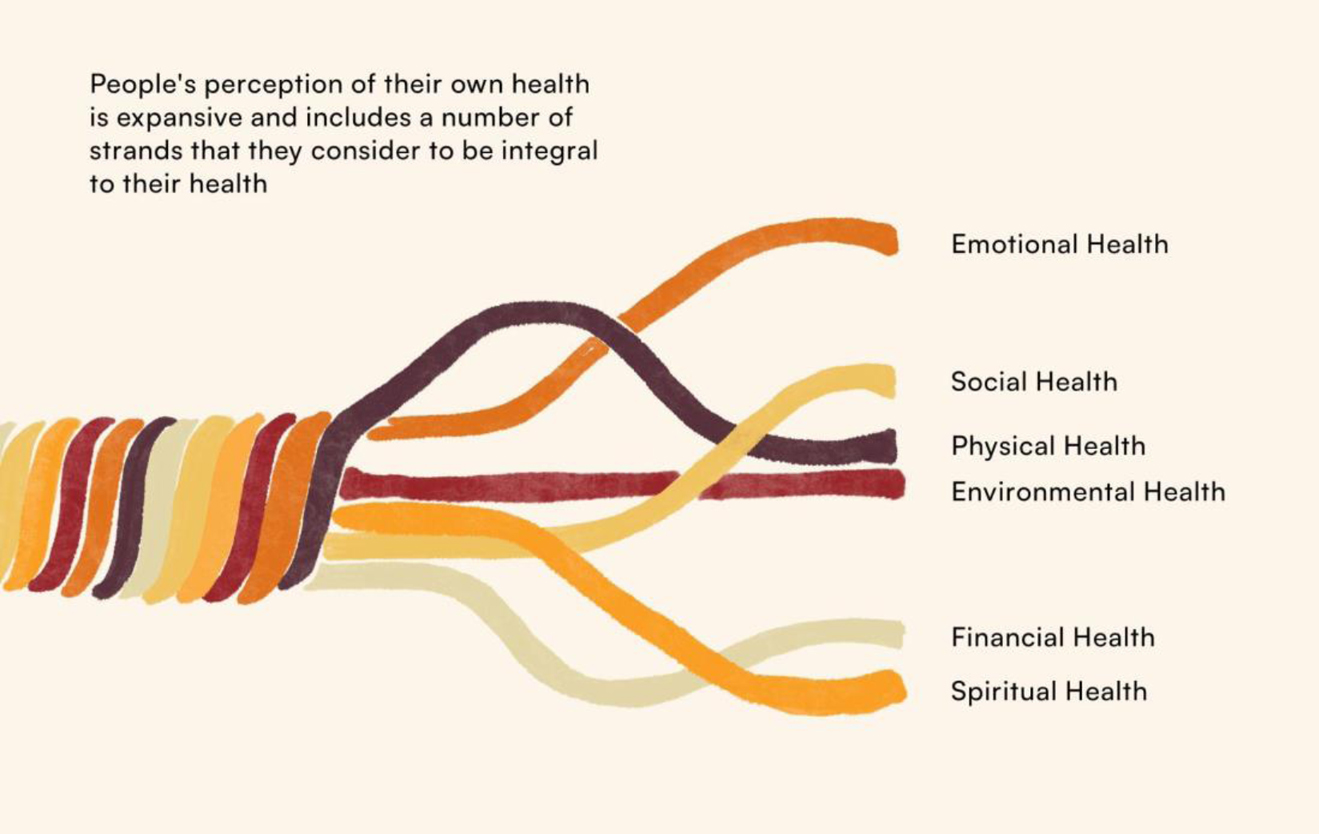
Figure 9: Health Strands. Illustration © Project ARC.
Once the strand based approach was articulated, it formed a core component of further analysis, centering the concerns of health seekers and helping identify points of friction between the health system and the people who use it.
Health Seeking Journey Maps
Mapping a user’s journey as they use a product or a service is a critical design thinking tool (Design thinking bootleg, n.d.). In most design-led public health projects this would likely form an integral part of the methodology and would typically involve mapping journeys of health seekers as they access healthcare services – understanding the barriers and enabling factors in these journeys as well as seeker’s experiences through various points in the journey (Bartlett et al., 2022). After detailed health seeking journeys from participants were captured in Round B, visual journey maps were created for ease of analysis. The journey maps broke a health seeking journey into clear constituent parts, which were often inflection points in these journeys, such as, for example, a diagnosis. The refined themes, which were updated after the clustering exercise in Round B were used as lenses to conduct preliminary analysis of these journey maps. However, the most effective method of analysis emerged when the team began to leverage the Strand Approach to analyze the health seeking journeys. This approach led to the final outputs of Project ARC, which are described in the next section.
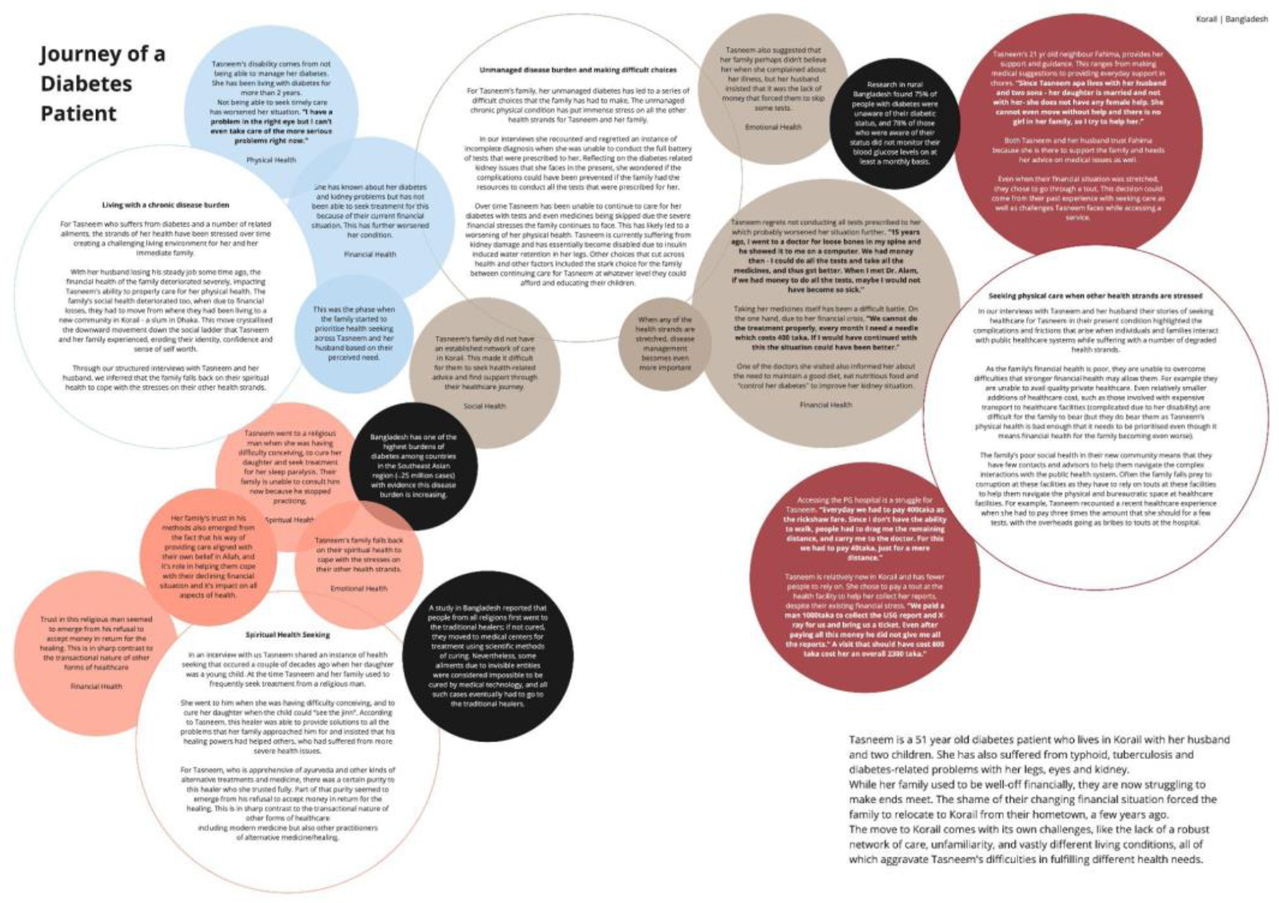
Figure 10. A sample of the journey mapping exercise. Screenshot © Project ARC.
OUTPUTS
As described earlier, the two core objectives of Project ARC were:
- To understand the experiences of health seekers as they interacted with a number of healthcare channels in order to identify frictions and opportunities (to improve their experiences), using the COVID-19 pandemic as an inflection point.
- To frame a set of design principles that are aimed at addressing the frictions that we identified from our research.
The two outputs of Project ARC discussed below each address one of these objectives.
Frictions
Using the Strand Approach, inflection points in health seeking journeys were analyzed to better understand the sources of frustrations (and at times, satisfaction) of health seekers, which could just as easily emerge from stresses in their financial health, social health, spiritual health as their physical health. These frustrations and failures were identified, categorized and clustered. These clusters were then labeled and connections between them were explored. What emerged was essentially a set of Frictions – gaps between health seeker expectations from the healthcare system, and what providers (primarily public health but even other types of providers such as private healthcare providers or traditional practitioners) were willing and able to provide them. Apart from being barriers, these frictions, perhaps more importantly, are also opportunities for interventions and innovations. These frictions fall within two broad and interrelated buckets of the typical health journey and the [lack of] enabling factors that contribute to the success [failure] of the health journey. They are briefly described below.
- The health journey:
- Awareness & Knowledge
The health system is often equipped to recognise a patient only after a successful diagnosis and patients are left to navigate the initial stages of their journey with minimal formal guidance. - Accessing the system
Through a healthcare journey, a health seeker has to make important financial, emotional, social, and spiritual decisions and sacrifices that have consequences on their health and the health of their families. These decisions take the form of ‘tradeoffs’, where certain strands are prioritized over others. While seekers are expected to make multiple trade-offs in favor of their physical health, they may perceive risk differently than their health providers. - Adherence & Maintenance
Upon diagnosis, seekers with serious ailments embark on an emotional transition from seeker to long-term patient, which is often a daunting experience for the seeker because of the trauma they experience from the diagnosis. Despite this, they are required to make this transition swiftly and without time and support.
- Awareness & Knowledge
- [Lack of] enabling factors:
- Dialogue/Trust/Understanding
The absence of dialogue can lead to an understanding gap, which over time can result in reduced trust in the health system. This becomes a vicious cycle that compounds over time. As a consequence, seekers may be left feeling confused, disempowered, ill-equipped in managing their own health journey, and unable to deal with their side effects. - Social Networks
Patients are part of an expansive social network, which includes family, friends, neighbors and non-formal health providers among others. By failing to leverage this network of care in a patient’s treatment, the system does not equip existing care-givers with information and skills that could improve a seeker’s health journey. - Intermediaries
Seekers need various forms of support to physically, emotionally and financially navigate a complex, at times bureaucratic public health system. While there is a large demand for this, the lack of formalized roles or solutions means that this support is provided largely by unregulated actors, such as touts or pharmacists, who are accountable neither to the seekers nor the system.
- Dialogue/Trust/Understanding
Design Principles
Design Principles are a set of fundamental positions used to guide the design process; they are not mere suggestions of activities but assertions that guide the designer to more effective outcomes (Mattson & Wood, 2014). Some scholars have added that “principles are not simply a listing of goals but rather a set of methodologies to accomplish the goals” (Anastas & Zimmerman, 2003). For ARC it is important that principles help provide a pathway for public health systems actors and other stakeholders in global health to arrive at better, more user centered health systems in the future.
The ARC team framed design principles ostensibly to address the frictions. However, as is discussed below, these principles were also aligned with objectives of public health systems. In this exercise the ARC team relied on an extensive literature review of existing innovations both within public health systems as well as those outside of it. Further, the team also sought inspirations from hacks that communities and individuals themselves arrive at to overcome frictions they face in accessing and receiving healthcare.
Digital strategies will play a critical role in strengthening health systems and they have been formally recognized as a strategy to help meet the Sustainable Development Goals and universal health coverage targets. However, our principles also reflect the limitations of digital strategies and the crucial role of in-person efforts in healthcare, particularly for the vulnerable. This recognition was formalized by the WHO in its 2019 guidelines and recommendations on digital interventions for health system strengthening (Recommendations on digital interventions, 2019). The guidelines, “urges readers to recognize that digital health interventions are not a substitute for functioning health systems, and that there are significant limitations to what digital health is able to address.” Research evidence from ARC underscores this, and our principles provide a necessary provocation for developing a hybrid phygital approach to health systems in the future; striking the right balance between digital and in-person efforts will be key in road mapping the health systems of the future. As such, the diagram below presents “Everything is Physical; Everything is Digital” as the central provocation.
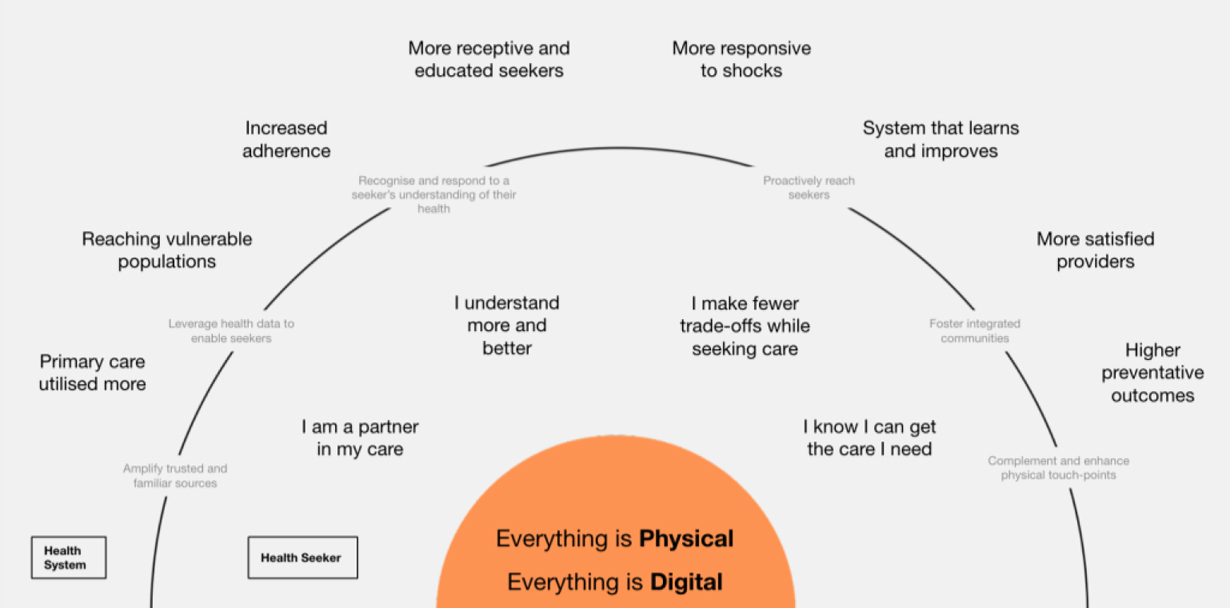
Figure 11. Design principles, patient needs, and health system outcomes. Illustration © Project ARC.
The innermost arc around this provocation presents a distilled version of the learnings from Project ARC regarding health seekers’ needs and expectations from health systems. Briefly these include:
- I understand more and better, which reflects the needs of health seekers to better comprehend and evaluate diagnosis, prognosis and treatment regimens when seeking care. It also reflects their need to understand their options for keeping healthy and preventing disease.
- I make fewer trade-offs while seeking care, which reflects the need of health seekers to consider and address stresses in all their health strands and their expectations of healthcare options that seek to minimize conflicts between their physical health and their other strands of health.
- I am a partner in my care, which reflects the need of health seekers to actively engage in their own health journey and feel a sense of agency. This also reflects the need that many health seekers express to involve their informal care networks in their health journey, which may include their friends and family but can also include neighbors and other members of their community.
- I know I can get the care I need, which reflects the need of health seekers to be aware of and trust the healthcare options that the healthcare system (particularly public healthcare) makes available to them.
The outermost circle in the diagram above represents the positive outcomes that health systems are likely to observe when the needs of health seekers (represented by the innermost circle) are met. These outcomes are self-explanatory and loosely tied to the health-seeker needs.
The space between the two circles is occupied by the design principles, which are articulated to form a bridge between the health-seeker needs in the innermost circle as well as the health system objectives in the outermost circle.
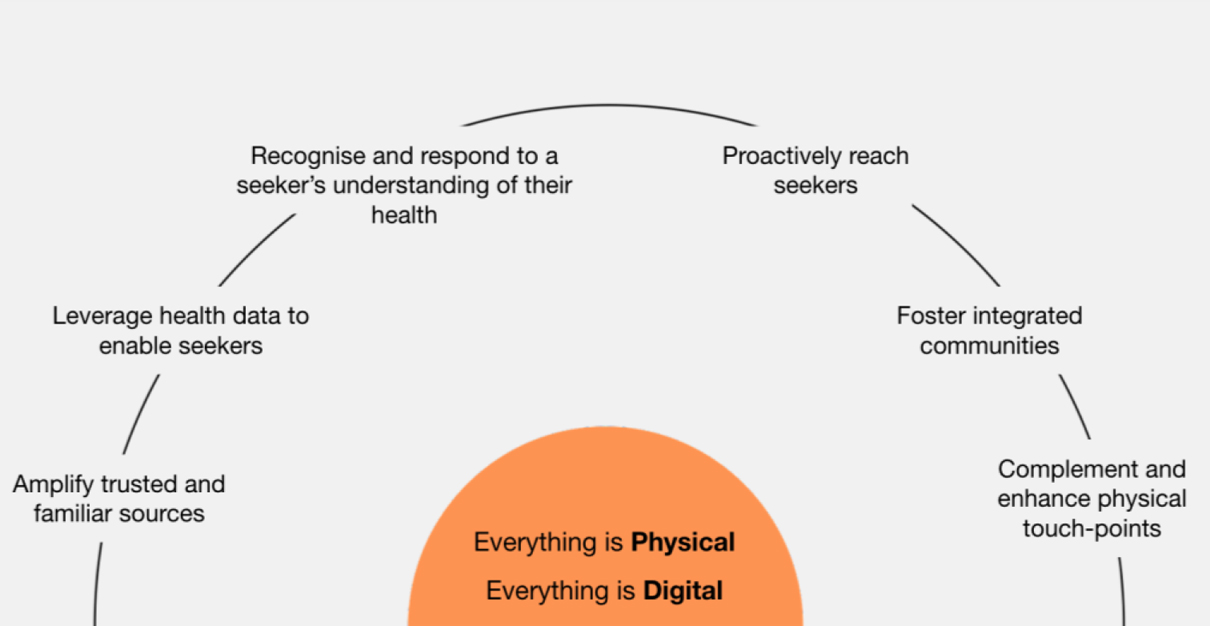
Figure 12. Design principles. Illustration © Project ARC.
These principles are briefly described as follows:
- Amplify trusted and familiar sources for health messaging, with appropriate moderation: Channels of communication that include trusted and familiar sources should be used to amplify health messaging and seeking but with appropriate moderation and regulation.
- Recognize and respond to a seeker’s expansive understanding of their health: All the strands that make up the idea of health for seekers should be acknowledged and considered during the course of their health journey.
- Leverage health data to enable health seekers to better understand and take control of their care choices: A seeker’s health information should follow her across all touchpoints of healthcare. This data, apart from contributing to the health system’s operational efficiency, should also be made available for seekers in formats that help them understand their health journeys better and have more control over their care choices.
- Complement and enhance, not replace physical touchpoints of care: Technology in health should seek to complement the in-person experience of health seekers, not aim to replace it.
- Proactively reach seekers and invite them to participate in their own care: The health system should be proactive in reaching health seekers and help them make the right decisions in their health seeking journeys. Furthermore, there should be an active invitation to health seekers to participate in their own care, seeding ways of engagement that creates more personalized, sustainable and trusting journeys of care.
- Foster integrated communities of practice between formal providers and naturally occurring networks of care: Formal care providers and naturally occurring networks of care should be facilitated to form an integrated community of practice to enable seekers to experience effective and mutually-flourishing relationships with their care providers.
These design principles connect core health seeker needs to the objectives of the health system, particularly the public health system. We hope that they would allow designers of health interventions and policy to better sync their approaches to health seeker expectations and needs, maximizing their chances of success.
Scenarios from the Future
As a next step in the project, the ARC team are developing ‘Scenarios from the Future’ – a design fiction exercise that leverages our findings to imagine what resilient health systems can look like, and explores the role of physical and digital infrastructures within these systems. This exercise is allowing the project team to bring together the strands of health and the points of friction in a more imaginative way, through storytelling.
CONCLUSION
The COVID-19 pandemic as an inflection point highlighted existing lacunae in public healthcare across the world by accentuating them. The pandemic further stressed social safety nets, financial capacity and mental health of individuals, especially among marginalized communities, and made visible how crucial these were in maintaining the health of individuals. Project ARC primarily focused on demand side challenges faced by health seekers, however our inquiry partially extended to healthcare provisioning as well, especially in the way it interacts with healthcare seekers, influencing their experiences. While the specifics of the challenges that health seekers face when accessing healthcare can be very local, we believe that our geographies of focus – Bangladesh and South Africa – provide an indicative understanding of the larger patterns of these frictions, especially in Low and Middle Income Countries (LMICs). A human centered design led approach, which included video ethnography allowed us to focus on the experiences of health seekers while accessing healthcare and how gaps in these experiences often lead to poor health outcomes.
Apart from challenges and barriers that individuals face while accessing healthcare, our learnings are also informed by community led innovations and workarounds, formal and informal that make individuals more resilient to shocks to their health. We also took into account public health interventions and programs that have worked by recognizing and addressing points of friction in accessing healthcare and adhering to treatment regimens. The design principles that emerged from these learnings are framed as guides for future health systems where these gaps can be addressed as far as possible, while keeping in mind the larger constraints around public healthcare that may continue to exist. The design principles are sensitive to the reality of digital efforts becoming increasingly crucial in complementing in-person care as health systems across LMICs seek cost effective ways to improve healthcare options, especially for marginalized communities. By recognizing the core needs of health seekers, identifying the frictions they experience while accessing healthcare, and framing principles for future health systems, we hope that we can contribute towards a more seeker centric healthcare ecosystem.
Romit Raj is a design researcher and a technologist. While his background is in humanities, he has spent a part of his professional career designing and building technology systems. More recently, Romit has immersed himself into design research at Quicksand leading HCD work in Public Health and Climate Change. Email: romit@quicksand.co.in
ACKNOWLEDGEMENTS
The authors of this paper would like to acknowledge work and support of the entire ARC project team:
The Bill & Melinda Gates Foundation
Tracy Pilar Johnson, PhD
Ipsos MORI
Sunny Sharma, Rebecca West, Heidi Hasbrouck, Sophie Mathison, Flora Ullah, Cassie Gardner, Sarah Bartle, and Gemma Spickernell
Global Development Technical Expert — Behavior Change
Anabel Gomez
Matchboxology
Cal Bruns, Cristin Marona, Nigel Branken, Owen Manda, Nomvuzo Khumalo, Mdu Simelane, Yvette Kruger, Sindi Washington, Kelvin Kaari. South Africa Partners: Brand ID, Aurum, and Culture Foundry.
Quicksand Design Studio
Babitha George, Romit Raj, Ayush Chauhan, Neha Singh, Ayushi Biyani, Reema Deshpande, Udeshi Basu, Aditya Prakash, and Rachit Shah
James P Grant School of Public health, BRAC University
Dr. Malabika Sarkar, Dr. Mrittika Barua, Humayra Binte Anwar, Jannatual Sumrina Hridhi. Suhan Ahmed Omi, Protyasha Ghosh, Shamsul Kabir, Kazal Dey, and Alifa Ahmed
Local Champions Network South Africa
Dr. Giovanni Perez, Metro Chief Director of Health, Cape Town
Mr. Russel Rensburg, Director, Rural Health Advocacy Project
Dr. Yogan Pillay, CHAI Country Director of South Africa, Senior Global Director for Universal Health Coverage
Dr. Nokwethemba Mtshali, Director, Health System Strengthening, Aurum Health Systems
Prof Jannie Hugo, Head of Family Medicine, Steve Biko Academic Hospital, University of Pretoria
Dr. Tlaleng Mofokeng, Special Founder/Vice Chair Sexual & Reproductive Justice Coalition SA, Author, Al Jazeera TV & Local Radio Host, Special Rapporteur UN, HumansRights Council
Prof Lucille Blumberg, Deputy Director, Nation Institute of Communicable Diseases
Prof Francois Venter, Deputy Executive Director, Wits Reproductive Health and HIV Institute, University of the Witwatersrand)
Local Champions Network Bangladesh
Mr. Anir Chowdhury, Policy Advisor, “a2i – innovate for all” Program of the Government of Bangladesh
Dr. Sayed Rubayet, Country Director, IPAS
Dr. Morseda, Director In-charge of Health, BRAC
Mr. Salman Khan, Office chief (Dhaka), Bidyanondo Foundation
Dr. Golam Mawla Baksh, Program Manager, EPI, DGHS
Mr. Sajjad Sharif, Managing Editor, Prothom Alo
Prof. Din M. Sumon Rahman, Dir. Office of Faculty Research and Office of Critical and Qualitative Studies, U-LAB
Dr. Shamima Akhter, Project Lead and Senior Technical Advisor, Thinkwell, Bangladesh
Dr. Sabina Faiz Rashid, Dean, BRAC JPGSPH
Dr. Samina Chowdhury, Project Management Specialist, USAID
NOTES
1. An individual’s care network typically involves their family, friends, neighbors and others who play a crucial role in keeping them healthy and helping them recover from illnesses. This idea is explored in more detail later in this paper.
2. The other being – informing the design of future health system interventions, which is described in more detail later in the paper.
3. The Global Fund supported programs across 106 countries reported disruption in 85% of HIV programs, 78% of TB programs and 73% of malaria as a result of the COVID-19 pandemic (Global Fund Survey, 2020).
4. For e.g., parents of newborn babies, people with infectious diseases, women with a need for family planning services, people needing catastrophic health hazard treatments.
5. A small advisory group was created in South Africa and Bangladesh. In parallel a global advisory group was also created. The purpose of these groups was to provide inputs both in refining our lines of inquiry for research as well as to be a sounding board for analyzed findings and insights. Members included representatives from grassroots and non-governmental organizations, government, public health, media and advocacy-centric organizations, and international development organizations.
6. Those who have not accessed the public healthcare system in at least 12 months.
7. Quicksand, India and Matchboxology, South Africa are practitioners of human centered design and design research, while Ipsos MORI, UK brought to bear their expertise in qualitative research, quantitative research and video ethnography. Similarly, partners brought together a number of analytical techniques that ranged from design oriented methods such as affinity mapping and journey mapping to video ethnographic analysis.
REFERENCES CITED
Alwang, Jeffrey, Paul Siegel, Steen Jorgensen. 2001. “Vulnerability as Viewed from Different Disciplines”. Social protection discussion paper series.
Anastas, Paul. T. and Julie. B. Zimmerman. 2003. “Design Through the 12 Principles of Green Engineering.” Environ. Sci. Technology 37: 94A–101A
Andrawes, Ledia, Tracy Johnson, Michael Coleman. 2021. “Complexity in Health: Can Design Help Support Interdisciplinary Solutions?” Global Health: Science and Practice. 9 (Supplement 2):S217-S225. DOI: 10.9745/GHSP-D-21-00222
Baah, F.O., Anne M. Teitelman, Barbara Riegel. 2018. “Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health—An integrative review.” Nursing Inquiry. 26:e12268. https://doi.org/10.1111/nin.12268
Bartlett, R., Tracy Robinson, Jennifer Anand, Fekir Negussie, Jessica Simons Smith and Jacqueline A. Boyle. 2022. “Empathy and journey mapping the healthcare experience: a community-based participatory approach to exploring women’s access to primary health services within Melbourne’s Arabic-speaking refugee communities.” Ethnicity & Health, 27:3, 584-600, DOI: 10.1080/13557858.2020.1734780
Braveman, Paula, Susan Egerter, and David R Williams. 2011. “The social determinants of health: coming of age.” Annual review of public health. 32: 381–398. doi: https://doi.org/10.1146/annurev-publhealth-031210-101218
Carroll, J. M. 2000. “Making use: Scenario-based design of human-computer interactions.” Cambridge, Mass. MIT Press.
“Design thinking bootleg.” n.d. Hasso Plattner Institute of Design, Stanford University. Accessed July 29, 2022. https://dschool.stanford.edu/resources/design-thinking-bootleg
Gkatzidou, Voula, Joseph Giacomin, and Lee Skrypchuk. 2021. “23. Fly-on-The Wall.” In Automotive Human Centred Design Methods. 76-77. Berlin, Boston: De Gruyter. https://doi.org/10.1515/9783110677515-024
“Global Fund survey: majority of HIV, TB and malaria programs face disruptions as a result of COVID-19”. June 2020. Global Fund. Accessed August 15, 2022. https://www.theglobalfund.org/en/covid-19/news/2020-06-17-globalfund-survey-majority-of-hiv-tb-and-malaria-programs-face-disruptionsas-a-result-of-covid-19/
“Global Strategy on Digital Health 2020-2025.” 2021. World Health Organization website. Accessed August 15, 2022. https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf
Hamada, Y. 2019. “Shadowing: What is It? How to Use It. Where Will It Go?” RELC Journal 50(3): 386–393. https://doi.org/10.1177/0033688218771380
Kittelsen, Sonja Kristine, and Vincent Charles Keating. 2019. “Rational trust in resilient health systems.” Health Policy and Planning. 34 (7): 553–557. doi: https://doi.org/10.1093/heapol/czz066
Mattelmäki, Tuuli. 2006. “Desing Probes.” University of Art and Design Helsinki.
Mattson, Christopher and Amy Wood. 2014. “Nine Principles for Design for the Developing World as Derived From the Engineering Literature.” Journal of Mechanical Design. 136(12):121403. doi: DOI:10.1115/1.4027984
Ozawa, Sachiko and Pooja Sripad. 2013. “How do you measure trust in the health system? A systematic review of the literature.” Social Science & Medicine. 91:10-14. https://doi.org/10.1016/j.socscimed.2013.05.005
“Recommendations on digital interventions for health system strengthening.” World Health Organization website. Accessed July 29, 2022. https://www.who.int/publications/i/item/9789241550505
“Social determinants of health.” n.d. World Health Organization website. Accessed July 29, 2022. ttps://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
Iba, Takashi, Ayaka Yoshikawa, and Konomi Munakata. 2017. “Philosophy and methodology of clustering in pattern mining: Japanese anthropologist Jiro Kawakita’s KJ method.” In Proceedings of the 24th Conference on Pattern Languages of Programs (PLoP ‘17). 12: 1–11.
Tanenbaum, T. 2014. “Design Fictional Interactions.” Interactions website. October 2014. Accessed July 29, 2022. https://interactions.acm.org/archive/view/september-october-2014/design-fictional-interactions-why-HCI-should-care-about-stories
Wrigley, A and A Dawson. 2016. “Vulnerability and Marginalized Populations.” In Public Health Ethics: Cases Spanning the Globe, edited by H. Barrett D, W. Ortmann L, Dawson A, Saenz C, Reis A, and Bolan G.. Chapter 7. PMID: 28590696.
