The COVID-19 pandemic changed many healthcare companies’ priorities and dramatically accelerated the drive towards increasingly virtual health care. Grand Rounds Health*, a healthcare startup, decided the time is now to launch its virtual primary care offering. It was assumed that a rural, lower-socioeconomic population would be more eager for, and best served by, virtual primary care, given their greater geographic distance from clinicians and other assumed access deficits. However, ethnographic research revealed that it was the urban, higher-socioeconomic population who both reported far more favorable experiences with remote care and more eager anticipation of virtual primary care. This is partly due to different technological experiences and ecosystems, but more directly due to differing trust in and agency with institutionalized health care. Ultimately, this case study reminds researchers that our experiences are shaped and limited by our social positions, and that we cannot know if the framing of our inquiry is adequate.
Keywords: Ethnography, healthcare, social location, socioeconomic status
CONTEXT
Prior to merging with Doctor on Demand*, Grand Rounds Health (GRH) was an employer-based, virtual healthcare company dedicated to their mission of “raising the standard of healthcare for everyone, everywhere.” Its primary offerings to members included expert second medical opinions, assistance with healthcare navigation, and facilitating virtual health visits with clinicians.
Creating a virtual primary care (VPC) experience was already on the long-term roadmap for GRH, but the COVID-19 pandemic—which necessitated an almost instantaneous, coordinated effort among clinicians and insurance companies to deliver virtual care of many kinds due to shelter-in-place—shifted many healthcare companies’ priorities and dramatically accelerated the drive towards increasingly virtual health care.
GRH considered primary care to be a mainstay of overall health. Research amply demonstrates that those who have a dedicated, longitudinal relationship with a primary care physician (PCP) have better health outcomes (Ganguli). However, primary care utilization in the United States is low—and trending lower.
Before actively designing a VPC experience, the design and product teams wanted to conduct exploratory research to address the following, foundational questions:
- What keeps people from engaging in primary care?
- How might virtual primary care address the primary care gap?
RESEARCH PROJECT DESIGN, METHODS, AND PARTICIPANTS
The main hypothesis going into the research was that the (United States domestic) rural population would be best served by, and more eager for, VPC, given their greater distance from clinicians and healthcare generally, and due to fewer options in rural areas for doctors who “are like/understand me,” with regard to ethnoracial identity, sexual orientation, gender identity, and other sociological and demographic statuses and signifiers. This hypothesis existed in theoretical contrast to an inverse assumption about the urban population: that closer geographic proximity to clinicians, and a greater diversity of clinicians to choose from, would render VPC less necessary or desirable.
Additionally, the rural population was considered, and the participant population selected, to be a rough proxy for the sizable number of blue-collar, working-class employees which GRH served; for example, industrial farm, retail, and warehouse workers. The urban population was selected to align with the higher-wage, white-collar GRH member population, such as Silicon Valley tech workers and middle- and upper-management employees in Fortune 500 companies.
We conducted remote, deep-dive interviews with the rural population—that is, relatively lower socioeconomic status (SES) and, with a majority living in rural and small towns, those who are most likely to have to travel considerable distances to a primary care provider, and/or for whom financial and geographic access may be problematic.
We conducted focus groups with the “urban” population: possessing a bachelor’s degree or higher (roughly half of the 36 focus group participants had graduate/advanced degrees), relatively higher SES, employer-provided health insurance, and urban/suburban residence. In short, for these participants, access to healthcare along multiple dimensions is not an issue.
Due to the logistical constraints of the pandemic we facilitated the focus groups and interviews online. This also enabled us to recruit nationally.
Across populations we discussed participants’ personal definitions and practices of “health,” their experiences with clinicians and institutionalized healthcare, and about their experiences with and hopes for virtual care.
Table 1. Research Design Overview
| Sampling | Homework | Interviews | |
|---|---|---|---|
| Urban | Above/well above national median annual household income of $63,000 36 people across 16 states; a diverse population of suburban/urban educated professionals with employer-provided insurance and access to healthcare |
Prior to the focus group discussions and interviews participants submitted individual answers to questions about social determinants of health, personal definitions of health and health practices, beliefs about primary care, and experience with virtual care. | Ten 1.5-hour focus groups with three or four participants in each group |
| Rural | At or below national median annual household income of $63,000 39 people across 23 states, all with employer-provided insurance, with a mix of demographic characteristics, varying levels of PCP use, and health status (excluding severe chronic conditions requiring in-person care) |
Individual or pair interviews, 1.5 hours |
A note on terminology: we define virtual primary care to be a combination of in-person services (labs, bloodwork, physical examination), and technology-based services (virtual/video-based consultations, messaging, scheduling, insurance navigation, health records, and provider identification). We refer to this set of services as VPC; it is important to note that participants were not given and did not use this definition so that their intuitive associations and mental model of virtual primary care could be uncovered.
FINDINGS
Not only were our original hypotheses debunked, they were found to be insufficient, in that they did not account for any kind of distrust of or skepticism in primary care. The urbanites far more enthusiastically anticipated the shift to a more, if not entirely, virtual care experience. Our rural participants were comparatively more skeptical, if not wary, of primary care, generally, and the potential for delivering it through virtual means.
Additionally, we found that socioeconomic status is the “meta” status that impacts other demographic signifiers and identities—specifically gender and ethnoracial identity—that in turn impact one’s personal calculus of the factors that affect engagement with primary care.
Socioeconomic status, not geographic location, has the greater impact on definitions of health, engagement with healthcare, and anticipation of virtual primary care. Thus, our two populations are no longer referred to as “rural” and “urban,” but “low SES” and “high SES.”
The differences between the low-SES and high-SES populations primarily lie in deeply entrenched beliefs about, and prior experiences with, institutional health care—and to a lesser extent, technological milieu— with the low-SES population likely needing far more persuasion to engage in institutionalized healthcare, and with virtual primary care, in the first place. These participants often do not see institutionalized healthcare, much less primary care, as valuable or trustworthy. Reducing access barriers (distance, time, cost) will not in itself persuade them to engage with institutionalized health care. Their low levels of trust lead them to see virtual primary care as a diminished form of in-person care; thus, even though they recognize the convenience offered by virtual care, they are unable to imagine a desirable future involving it. In contrast, the high-SES population was much more optimistic, and the healthcare futures they anticipated did not, unlike those of the low-SES population, involve dread.
Chain of Causation: Individual Determinants of Health Shape Engagement With Primary Care Across the SES Spectrum
A literature review conducted as the research was being carried out showed that structural forces are operational in healthcare:
- SES, gender, and ethnoracial identity all shaped healthcare experiences. (Gage-Bouchard, Shim, Springer, Timmerman)
- Social determinants of health help make sense of health infrastructures and outcomes (Braveman and Gottlieb, Marmot and Wilkinson)
We used both lenses to make sense of individual primary care behaviors, enabling us to spot patterns in personal accounts that correspond to patterns and structural forces identified in the literature.
In addition to these forces pertinent to a person’s social location and identity, our research revealed four individual determinants of health:
- Trust The degree of confidence that people have in doctors and the healthcare system
- Theory of Health How people define and manage their own health, and the role and value they assign to primary care
- Access Access members have to healthcare, and resources they have to spend on or engage with healthcare
- Agency The control (or lack thereof) people believe they have over their health
These individual determinants of health are the results of the social determinants inscribing themselves into individual psychologies and circumstances through encounters with the healthcare system and cultural narratives.
Taken together, these individual determinants of health explain primary care behaviors in both high- and low-SES populations. Though we observed clear patterns across the SES spectrum, it is important to note that ethnoracial identity, gender identity, and individual histories of socialization contributed to behavioral variation within each SES and identity cohort; SES and identity did not over-determine health outcomes and behaviors for our participants.
In summary, we propose this chain of causation:
SES, ethnoracial, and gender identities shape social determinants of health that produce individual determinants of health which drive and inhibit engagement with primary care.
Before we explore how high- and low-SES populations produce and experience the four individual determinants of health, we summarize how SES interacts with ethnoracial and gender identity in the context of healthcare:
Ethnoracial Identity
The impact of BIPOC identity on healthcare experiences maps pretty closely to that of SES. This is in large part due to historic and systemic discrimination against non-white Americans, leading to their over-representation in lower socioeconomic statuses.
Additionally, for the African American population, lack of trust in institutional health care also stems from historic abuses inflicted during notorious, unethical research experiments—and also from current, lived experiences.
Both our BIPOC population and many women, across the SES spectrum, voiced preference for a primary care clinician who shares their ethnoraical identity and/or gender orientation.
Gender Dynamics
High SES Men are less likely to exhibit stereotypical, hegemonic masculine traits and beliefs, and are more inclined to define health comprehensively. They are far more likely to engage with therapists and discuss the matter without stigma.
Low SES Men are far more likely to embody hegemonic masculine traits – particularly regarding their dedication to self-maintenance and individualism, which often translates into minimal use of, or disengagement entirely from, institutionalized health care (Springer and Mouzon). Women report, relative to our high-SES population, far more disrespectful treatment from healthcare professionals, such as not being taken seriously and having to endure far more unnecessary pain. Stories of dismissive, sexist behaviors from health care providers are more common as well.
HIGH SES: WELL-POSITIONED AMONG MULTIPLE DIMENSIONS TO EAGERLY ANTICIPATE VIRTUAL PRIMARY CARE
Among urban and suburban professionals with employer-provided health insurance, beliefs about virtual health care are changing quickly, and due to positive experiences with virtual care, overwhelmingly for the better. They experienced the evolution of virtual care in real time during the pandemic, over multiple appointments, with various doctors (dermatologists, pulmonologists, therapists, PCPs), and know that virtual care is in its infancy and will continue to improve. While the pandemic forced many to engage in virtual care for the first time, their experiences have resulted, in the main, in great success and satisfaction. Though there are a very few narrow, entrenched attitudinal and perceptual barriers to VPC—mainly the perceived inability to collect physical data (i.e., draw blood, take vital signs)—positive remote health experiences are paving the way for greater acceptance of VPC, and all agree that there is no turning back to exclusively in-person medical care.
Summary of High-SES Manifestation of Individual Determinants of Health
Trust The high-SES population trusts institutionalized health care and western medicine generally, and has a positive history of successful institutional interactions to draw from and build on. They also typically trust individual clinicians’ competence and diagnoses/assessments.
However, some doubt the ability of an overtaxed medical-industrial complex to deliver ideal health care. For example, participants often asked, rhetorically, “In a 15-minute meeting with a hard stop, and with all the patients my doctor sees, how can they really know me—or anyone?”
Theory of Health The vast majority of high-SES participants have a multi-dimensional theory of health. That is, health is not merely a physical condition (be free from pain, eat healthy foods, exercise often), but includes mental, social, emotional, and sometimes spiritual health as well:
“To me, being healthy means giving my body and mind everything they need to live and do the things that I need and want to do. Specifically, this includes exercising (I meet with a personal trainer twice a week and also like going for walks); eating a well-rounded diet (something I can struggle with); talking with my therapist; connecting with friends, family, and community (which is challenging during the pandemic); creating time for solitude (walks, baths, other quiet & low stimulation activities); and making time and space for creative expression (crafts, home improvement, etc.)”
Access The high-SES population has fewer material barriers to successfully engage in institutional healthcare. They also live in and are more comfortable with a modern, expensive tech ecosystem, thus having the devices, broadband, and mastery necessary for a successful virtual care appointment. The almost-overnight and universal shift to remote work helped to make the transition to virtual care more of a small pivot than a giant leap. In the main they also have more flexible work schedules to accommodate health appointments that occur during the workday, more leverage/permission to take time off if needed, and are better able to secure and afford child care during medical visits.
Agency This population has been socialized from a young age to be informed, empowered self-advocates who feel entitled to ask for clarification or suggest alternate medications or courses of treatment (Lareau). They have the interpersonal savvy and medical literacy to communicate effectively with clinicians and create positive outcomes. They are confident and competent when navigating institutional bureaucracies. They have experienced the system work for them (Gage-Bouchard, Shim).
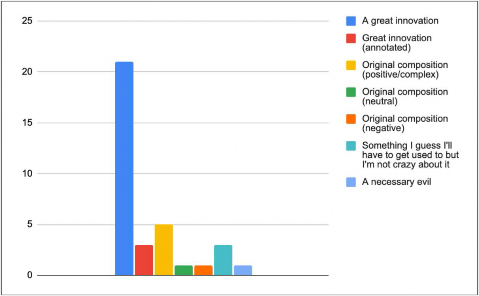
Figure 1. High-SES Perceptions of Virtual Health Care. As illustrated in the above table, the vast majority of high-SES participants feel that virtual health care is a great innovation; this played out in detail in the focus group conversations as well.
The main reasons for their effusive assessments include:
Convenience Busy, white-collar professionals deeply appreciate frictionlessly popping in and out of a virtual care appointment, thus avoiding the hassle involved in taking time out of the workday to commute to and from the doctor’s office, find parking, and possibly have to arrange for child/family care. And even if one has to wait a while for the doctor to appear and the appointment to formally begin—no worries, one can just keep working on their laptop until the moment it commences.
Physical and psychological safety While most appreciated being free from the stress and potential health hazard of being in close quarters in a waiting room with other, possibly sick people, many also mentioned, in their individual activities and in the focus group discussions, that virtual visits are preferred since home is also a safer psychological space:
“I currently see my psychotherapist weekly via video chat, and I’ve also met with my primary care doctor in the last year via video chat. Considering my primary care visit specifically, I would give it an A, I think. There wasn’t anything that especially thrilled me about it, but it was really helpful to be able to schedule a conversation with minimal disruption to my workday and to see and talk to my doctor from the comfort of home. I didn’t feel like the conversation was hindered at all by video, which is odd because I sometimes feel like other conversations are (work, friends and family). I guess I was perhaps more relaxed because I wasn’t in an unfamiliar exam room.”
LOW SES: VIRTUAL CARE HAS BOTH PROMISE AND PERIL
The low-SES population often does not see primary care as being helpful enough to be worth engaging with in the first place—much less virtual primary care. Even when access is not a problem, they may still not believe it is worth it to go to a PCP due to:
- Lacking trust (in the system, fundamentally; in the doctors to whom they have access)
- Not believing that PCPs are the people who can do something about ill-health
- Not believing that anything can be done to help them or that they have control over their health
Under these conditions, the low-SES population conceives of virtual primary care as having both promise and peril. Their interest in virtual primary care is measured and conditional.
Trust People in the low-SES population expressed distrust of both doctors and institutional healthcare more often than the high-SES population. They believed the healthcare system prioritized profits over providing care for people, and that doctors—however well-meaning—were therefore subject to its pressures and unable to or uninterested in treating people well.
Many people we interviewed spoke vividly about being ignored, disrespected, and discriminated against. They described medical professionals ignoring their knowledge of their own bodies, not taking their pain seriously, assuming drug-seeking and other negative behaviors based on their (apparent) social class, speaking dismissively and rudely, and conducting procedures over their objections or counter to their preferences. Making all of this worse are doctors with very limited time to spend with patients—leading to oversights and bad diagnoses. Occasionally, this led to damage to their bodies or put them in debt.
As a result, low-SES people saw themselves as being at the mercy of powerful institutions, with no one on their side or watching out for them. Faced with seeking medical care, participants frequently said that they would rather put up with what they believed to be temporary pain and ill-health than risk financial catastrophe and the possibility of further damage to their health. Participants described inheriting these attitudes from their parents, suggesting that seeking primary care is a socialized behavior. Unless exposed to other perspectives through education or culture, younger generations might continue to model their care-avoidant behaviors after their parents.
Access The researchers initially conceptualized access in terms of distance from primary care providers or healthcare facilities. In reality, low-SES people, both rural and urban, were comfortable driving considerable distances in order to reach the care they needed, being accustomed to long drives. Instead, the participants conceived of access barriers more in terms of other kinds of constraints on time and money, such as wait times and other demands on their finances.
Central to this is a terror of facing catastrophic costs they had no say in deciding whether to incur. According to many participants, many of their doctors and medical professionals often have no idea of the costs of the procedures or the impact it may have on them. Many even described being pressured into procedures whose costs they were not informed of beforehand.
Many of our low-SES participants saw healthcare as competing with other expenses. Having to decide whether to spend money on survival or health care, most choose survival. Parents having to decide whether to spend healthcare money on their children or themselves would usually decide to spend it on their children; whenever possible, they would avoid spending money on their own health in order to reduce the burden on the family. Given the precarity of their income, most low-SES parents were optimizing for cash flow and ongoing availability of money. In contrast, high-SES parents decided to make greater investments into their own health so that they “could be there for my children and grandchildren”, a long-term positive vision that low-SES parents rarely expressed.
These kinds of choices appear to be deeply informed by cultural narratives: of rugged self-reliance, wanting to not ask for help, and valorizing self-sacrifice for one’s kin. These were often deeply intertwined with narratives of masculinity; several participants talked about themselves or partners as “country men” who could “solve any problem with duct tape”.
For those low-SES people working multiple jobs, healthcare services are often unavailable during their free hours. Many participants did not have sufficient discretionary time off for healthcare visits, and had to negotiate time off with their managers, colleagues, and corporate bureaucracy. Coordinating time off with provider availability was often difficult enough that participants simply put off care visits or ignored issues entirely. Thus, they strongly appreciated how virtual care could allow them to see a doctor “at 11pm, after I’ve put my kids to bed”. In contrast with a narrative often espoused by high-SES people, these participants did not talk in terms of their time being valuable, but as being limited. While they clearly expressed a desire for it, there was no corresponding sense of entitlement to efficient and convenient visits.
Theory of health Low lifetime exposure to institutionalized healthcare due to lack of access and low trust leads to low-SES populations having a theory of health much more centered around the management of pain, as compared to the high-SES population’s conception of health as holistic and expansive. Pain management itself was influenced by narratives of agency: participants often described waiting it out until it got bad enough that they couldn’t keep going about their day anymore, justifying it with “it’s good for my body to tough it out”, or “taking medication weakens the body”.
Healthcare providers appeared to be doing little in the way of educating their patients; participants described how most of their interactions with doctors were rushed, with the doctors only giving them cursory attention. This meant that low-SES people received little, if any, actionable advice during annual checkups, being only told that their health was good or poor without any direction on how to maintain or remedy it. This contributed to a reduced interest in seeking primary care, because, as one of our participants put it, “I know I should be eating better and doing exercise. Why would I spend money on a doctor for them to tell me what I already know?”.
Given this situation, alternative providers of healthcare or healthcare information — chiropractors, people in the media, medical professionals in the family — become trusted sources that inform their theory of health.
Agency Low-SES people often had a history of being not given agency in institutional care settings. Trust-sapping experiences of being disrespected or ignored meant that, for these people, engaging with healthcare often leads to poor outcomes, leading to a belief that primary care is ineffective, and even that their health-seeking actions have no effect. Some participants internalized these experiences to mean that they were beyond help, and that they were destined to struggle and suffer by themselves. As one African-American participant concluded after having been prescribed blood pressure medication that was known to have dangerous side effects for AA men: “I really don’t think there’s a doctor out there that can help me, but that’s just my mindset.” Few participants possessed the ability to push back against a healthcare professional’s advice, ask questions, or request adjustments, in contrast with high-SES people who assumed asking questions to be both normal and essential to achieving good outcomes.
This perceived inability of low-SES people to positively affect their health is also informed by a pain-centered theory of health, which gives no structure to health-making activities or habits. Many participants took this to mean their health was essentially out of their control, and that it was no use consulting a primary care provider. When they did take action, it was often informed by alternative sources of health information and personal experimentation – not solely by their primary care provider.
Low-SES People Have a Comparatively Lesser Degree of Anticipation for Virtual Primary Care
“Well, I know I did a lot of teleconferencing with my doctor after I had my surgery. And I guess what made it impersonal was it was kind of weird because I was cut from, basically from my belly button down midway of my vagina and I had to stand up in front of him. So he could see the incisions and I’m like, how do I not know he has someone on the right side of the camera that I can’t see or someone on the left? And then he’s like looking around and not, I don’t know. It felt like he wasn’t actually paying attention to me. I don’t know. So when they did offer, when they said, do you want to make the drive and come see us in the office? I always took that opportunity.”
Given their history of poor experiences with institutional health care, mental models that de-center primary care, and scarce resources, low-SES people have only a measured interest in virtual care.
The main reasons for this are:
Poor first impressions Low-SES people’s experiences with virtual appointments has been far more mixed/less positive than the high-SES population. Many participants first used virtual care during the pandemic, and they experienced what they considered to be a more limited or degraded form of care. As medical practice adapted quickly to cope with the constraints placed by the pandemic, the doctors our participants consulted were stressed and unable to offer more than cursory support. It is also possible that the low-SES population was then not yet acclimated to Zoom and similar platforms, and considered it to be a sub-par interaction.
Psychological unsafety and impersonal interactions Low-SES people we spoke with felt strongly that virtual interactions were more impersonal and less emotionally resonant than in-person interactions. Many feared that talking through a screen meant that the doctor would be free to pay even less attention to them than they already did, and that biases would be exacerbated. Being present in-person, for them, was seen as a way to be taken seriously, and gauge both the quality of the interaction and the character of the healthcare provider accurately.
Lower quality of care Low-SES participants—even those who had some limited VPC experiences—were concerned that consultations through video would be lower quality. Though this concern is partly about the quality of the cameras on their devices and bandwidth restrictions, it is more about the small viewing window limiting the doctor’s ability to really observe their bodies closely and as a whole and note symptoms accurately. Video consultations were seen as potentially shifting the reporting burden further on the participants. Current primary care models have established that a consultation necessarily involves gathering vitals and other bodily data; participants instinctively decided that VPC, lacking these sorts of physical interactions, must necessarily be less effective than in-person care. Unlike our high-SES participants, these people did not express an interest in smart watches, health apps, and other medical technologies as part of their desires for improving primary care. Technology was rarely seen as an opportunity for better care.
Loss of agency Thus, seeing virtual care as “less than” in-person care, many low-SES participants expressed a fear of being trapped in systems that further limit their care options. They were concerned that virtual care offerings were just another way for healthcare providers to cut costs, and to take away forms of care that felt trustworthy.
At the same time, they were also appreciative of its potential benefits:
Convenience Free hours for many low-SES people often don’t align with provider availability. Many low-SES people we spoke with identified the potential for VPC services to be available during their non-working hours. Many also thought that they would not have to choose between childcare and seeking primary care for themselves, and also that VPC would make it a lot easier to have a consultation regarding their children without having to set aside the time and effort to drive them to the doctor’s office. Also appreciated was the uncoupling of gathering blood and vitals from the doctor’s consultation—some participants suggested that the doctor’s limited time for review could be supplemented by more time with a medical professional who could explain the recommendations and answer questions in more detail.
Psychological safety Low-SES participants talked about a virtual primary care visit being easier to leave if they found it unpleasant or not serving their needs. As one person said, “If I don’t like it, I can just shut the laptop”. Walking out of an appointment is seen as the primary form of agency they do have in healthcare settings; VPC makes that easy. Participants noted that a virtual consultation or provider would require a lesser investment in time and travel, thus making it easier for them to change their minds and seek another provider. In addition, spouses and caregivers also appreciated how VPC makes it easier for them to participate in the care process for their loved ones, primarily by accompanying them on visits or consultations.
In summary, our low-SES population did see some benefits of virtual care, but their anticipation was tempered by their mistrust of institutional healthcare. In addition, in comparison to high-SES people, these participants conceived of virtual care as comprising a more narrow set of experiences centered around a visit to the doctor.
Summary of Key Differences Between the Low- and High-SES Populations
Personal Theory of Health/PCP role
High SES Personal health is multidimensional: physical, mental, social, perhaps spiritual. One’s PCP is assumed to be a partner in and vehicle for furthering personal health, which is in theory a proactive endeavor—though people admit to falling short of the proactive ideal.
Low SES Often there is no coherent theory of health, but when there is, it is frequently limited to exercise and diet. People may or may not have a PCP. Indeed, they may not be engaged with the institutionalized healthcare system at all: PCPs are not assumed, easily accessed allies in pursuit of health. In the main, people engage in institutionalized healthcare far more reactively.
Prior History/Experience with Health Care
High SES There is very likely a lifelong, positive history of institutionalized health care experiences, with multiple specialists, to draw from. If one is dissatisfied with the quality of healthcare one is receiving, one feels empowered to advocate for oneself or to seek alternatives. If one has a negative experience with an individual doctor, dissatisfaction/blame lies squarely with that specific practitioner: disengagement from institutionalized health care is rarely considered.
Low SES Far more negative health care experiences were discussed, particularly regarding pain being taken seriously, pain medication being prescribed (or not), and participants feeling fully heard and respected. Participants are comparatively more wary of institutionalized health care, and are more likely to have been disengaged from institutionalized health care entirely for extended time periods.
Assessment of experience with virtual care
High SES Virtual care experiences have been overwhelmingly positive, mainly due to convenience, physical safety, and psychological comfort. Just as important, but more invisible, are the devices and infrastructure enabling the technically smooth experience. The main barrier to greater acceptance of a VPC experience is belief that insufficient bodily data can be obtained through remote appointments, though most report being comfortable with new and emergent technologies to bridge this gap. An in-person appointment is still desired for circumstances when human engagement is seen as required (a medical emergency, a broken leg, blood being drawn).
Low SES Assessment of virtual care experiences is far more mixed, due to trust issues (the doctor is looking away/at another screen; is someone else in the room with the doctor as I show my scar?), belief that insufficient bodily data can be obtained through remote appointments, less value placed on “convenience” per high-SES metrics, and entrenched willingness to drive, even long distances, to a local, in-person doctor. Lack of broadband access, old and hand-me-down devices, and relatively less familiarity with Zoom and similar platforms exacerbate the poor experience.
Qualities desired in PCP
High SES The “most important” qualities PCPs should embody include taking the time to really listen, empathy, charismatic bedside manner, the willingness and connectedness to send one to a specialist when needed, and restraint from over-prescribing medications—and, conversely, from prescribing medication as a default.
Low SES There are differences between the two populations regarding the experience of “being heard.” Most low-SES participants mentioned the desire to be heard/that doctors need to listen. However, high-SES participants predominantly stated that being “listened to” means not being rushed, or being granted sufficient time to fully discuss their questions and concerns. For low-SES participants, being “listened to” far more often meant being “respected,” in addition to not being rushed.
Attitudes towards mental health
High SES Engaging in talk therapy is seen as normalized, proactive personal maintenance and self care. Little if any stigma around discussing mental health maintenance was perceived.
Low SES Mental health care is far more stigmatized—and often not sought until people are confronting a crisis or at a breaking point. Religious institutions are more likely to be seen as the best source of mental health care.
DESIGN IMPLICATIONS
At the time of this writing we are working with the GRH+DOD product and marketing teams to craft an effective VPC experience and to compose attendant, compelling messaging. The initial hypotheses about to whom VPC would appeal, and why, have been debunked, and we are moving forward with greater clarity and confidence. Our research is informing the design of our VPC experience—and more.
Personas The primary deliverable resulting from this research is the Virtual Primary Care Personas, which are being used throughout GRH+DOD, and more expansively than for just VPC design. The personas are
- facilitating understanding about GRH’s member population to Legacy Doctor on Demand and Included Health teams as our companies and cultures merge*
- informing the value propositions for marketing positioning statements
- being leveraged to design conversations for the digital assistant
- being used to represent the customer/patient population when designing digital tools for our clinical and care teams
In addition to considering the needs, motivations, and beliefs of the personas, GRH+DOD must also consider these implications and principles for design:
Address all four individual determinants of health. It is clear that simply creating a usable and accessible VPC service only serves the most well off and technically proficient people, and risks alienating those who will most benefit from increased engagement with primary care. To succeed, GRH+DOD must address all four factors when designing their VPC service:
- Earn trust (and evaluate interactions knowing a deficit of trust may be present).
- Speak to the user’s current theory of health, help enrich their understanding of their health, and help evolve it to be more holistic (especially expanding it to include behavioral and mental health).
- Empower people to act, knowing that mistrust, hegemonic masculinity, a lack of socialization into health practices, and cultural background will make this more difficult for some.
- Make the service available to people working a range of hours during the day or week, ensuring that people face no surprises and that they have agency over every interaction with the doctor and all prescribed courses of treatment.
Design for the medium Understanding that video interactions read differently depending on users’ socialization with technology and the trust or mistrust they may have, GRH+DOD needs to train its clinical care providers to adapt their behavior for video-based interactions. Care will need to be taken to signal empathy, respect, and attentiveness, or patients might infer that the provider does not care and/or is not competent. Secondly, the service must be usable with low-quality cameras, older devices, slower bandwidth, and limited skill with technology.
Meet people where they are in their journey People will be in various degrees of readiness and ability to engage with both primary care and VPC. GRH+DOD will need to identify factors that have shaped a person’s past experience with healthcare, understand their present needs and abilities (including those related to technology use), and compassionately empower them to change in positive ways. This also means that different sub-populations will have different success metrics, and they will progress towards ideal primary care and health behaviors at differing rates.
Design with relationships in mind Though our research focused on personal health-making behaviors, it was very clear that the majority of people at both high- and low-SES have personal relationships that inform their primary care behaviors—in the household, the family, and at the workplace. Thus, it will be important to not only design for the individual personas but also make it easy for people they trust to be involved in or accompany them in primary care experiences. Doing so will ameliorate trust deficits, create psychological safety, and increase the likelihood of outreach and marketing efforts succeeding.
PROVOCATIONS
Who creates/anticipates the future? For whom is the future designed?
Our two populations have strikingly different anticipations of future technology and experiences—one optimistic, one filled with dread—each strongly determined by their position in society, and the structural forces acting on them.
Why was the dread invisible to the experience designers?
The GRH+DOD team is of the high-SES cohort, whose life experiences reinforced narratives that suggest optimism. Many, if not most, have never faced the challenges and barriers the low-SES population does, so they could only anticipate the benefits of the healthcare future they are creating. They assumed that primary care was universally desirable, and did not expect that people would question its fundamental value. When this assumption was shown to be false, it changed not only the marketing, outreach, intake, and design goals, but also affected estimates of adoption rates for a VPC product, and for which populations.
We submit that this case study demonstrates how operating ethnographically is valuable. By explicitly investigating and being open to aspects of experience that are beyond the immediate concerns of our product teams, by helping us see what we have been blind to, we are able to identify significant risks and avoid strategic errors…but only if we are able to acknowledge that our gaze is limited when we begin. In this project, if we had only investigated virtual primary care, or had only investigated current members, or had not tried to probe to a level where we could see structural forces operating over time, we would not have uncovered how deep of a trust deficit exists. An inquiry limited to understanding needs around virtual primary care would not have uncovered these underlying beliefs that would limit the use of even the most well-designed and usable VPC products.
This case study is also a reminder that our experiences are pervasively being shaped by our social position, and that we cannot know if the framing of our inquiry is adequate. In other words, representation matters, and black/POC/trans/disabled activists are right that systemic forces render their experiences invisible to people with power. This is often cited as a reason to have a diversity of people on the team. However, people from underprivileged backgrounds often face pervasive biases and other barriers, and team culture may prevent them from being able to speak to their experience, or challenge assumptions (see Luckie, and Wachter-Boettcher). Countering this invisibility requires a commitment to including their perspectives when framing the research, including them in the research sample, and shaping the inquiry with awareness of structural and systemic forces that shape human experience.
Finally, we should assume that futures may not be anticipated the same way across our stakeholder population, and therefore should explicitly inquire into both desire and dread. Asking not only about who might benefit from a technology and how, but also who might lose — perhaps using frameworks like McLuhan’s tetrad of media effects (McLuhan and McLuhan) — can help expand our gaze as practitioners, and help make sense of the societal impact that technology is likely to have.
Marie Mika is a sociologist and Staff Researcher at GRH+DOD, leading virtual primary care research. Previous clients include Ford, Genentech, Google, Hyundai, and Whirlpool, and she is proud that her studio’s game won Google Play’s 2019 Best of Casual Games. Please feel free to contact me at marie.mika@grandrounds.com
Arvind Venkataramani leads design research for clients at SonicRim but actually creates for them tools and containers for learning, discovery, and collaboration. He dislikes third-person bios and would rather you talk with me about systems, decolonization, discourse traps, mindfulness, the sociological eye, and eldritch horrors of the modern era. At arvind.venkataramani@gmail.com
NOTE
This research project was launched in December 2020, prior to Grand Rounds Health merging with Doctor on Demand in early 2021 to form what is presently and temporarily named “GRH+DOD”. The study was designed with Grand Round Health’s member population, business model, and goals in mind. Therefore, this Case Study will refer to Grand Rounds Health, rather than GRH+DOD, unless explicitly noted. Additionally, GRH+DOD acquired Included Health in May, 2021.
REFERENCES CITED
Braveman, Paula, and Laura Gottlieb. 2014. “The Social Determinants of Health: It’s Time to Consider the Causes of the Causes.” Public Health Reports 129 (1_suppl2): 19–31. https://doi.org/10.1177/00333549141291S206.
Gage-Bouchard, Elizabeth A. 2017. “Culture, Styles of Institutional Interactions, and Inequalities in Healthcare Experiences.” Journal of Health and Social Behavior 58(2): 147-65.
Ganguli, Ishani, et al. 2020. “Declining Use of Primary Care Among Commercially Insured Adults in the United States, 2008-2016.” Annals of Internal Medicine doi:10.7326/M19-1834
Lareau, Annette. 2015. “Cultural Knowledge and Social Inequality.” American Sociological Review 80(1):1–27.
Luckie, Mark S. 2018. “Facebook Is Failing Its Black Employees and Its Black Users.” Facebook Is Failing Its Black Employees and Its Black Users (blog). November 8, 2018. https://m.facebook.com/nt/screen/?params=%7B%22note_id%22%3A3121422367961706%7D&path=%2Fnotes%2Fnote%2F&_rdr.
Marmot, Michael, and Richard Wilkinson. 2005. Social Determinants of Health. OUP Oxford.
McLuhan, Marshall, and Eric McLuhan. 1992. Laws of Media: The New Science. Toronto: University of Toronto Press, Scholarly Publishing Division.
Shim, Janet K. 2010. “Cultural Health Capital: A Theoretical Approach to Understanding Health Care Interactions and the Dynamics of Unequal Treatment.” Journal of Health and Social Behavior 51(1): 1-15.
Springer, Kristen W., and Dawne M. Mouzon. 2011. “Macho Men and Preventive Health Care: Implications for Older Men in Different Social Classes.” Journal of Health and Social Behavior 52(2) 212-27.
Timmermans, Stefan. 2020. “The Engaged Patient: The Relevance of Patient-Physician Communication for Twenty-First-Century Health.” Journal of Health and Social Behavior 61(3) 259-73.
Wachter-Boettcher, Sara. 2017. Technically Wrong: Sexist Apps, Biased Algorithms, and Other Threats of Toxic Tech, ch 2. 1st edition. W. W. Norton & Company.
