Case Study—This case study highlights the value of exploring the reality of having and treating psoriasis. Its aim is uncovering why it is that, despite treatments being available that offer transformative results, people with psoriasis can continue to live in isolation and with feelings of shame. If clear skin alone isn’t enough, what is it that can help create a sense of well-being? Even undertaking a piece of work like this represented a significant step forward for the pharmaceutical industry where, historically, investing in this kind of deep patient insight work hasn’t been common and where getting buy-in to the outputs is far from certain. How can sight lines be created and developed, particularly from physicians to patients? Explored in this case study are not only the ethnographic and other methodologies used, but also: some of the challenges in bringing together this encompassing piece of work; the strategies and efforts made to ensure that core audiences engaged with the research; how minds were changed inside the client’s business, established ways of working challenged to appreciate the value of human-centred insight; and, the real world impact of the work.
Keywords: Ethnographic Case Study, Culture, Narrative Shifts, Co-creation, Prototyping, Design Thinking, Behavior Change, Health, Psoriasis
INTRODUCTION
Grief, stress, overwork, crumbling relationships. These and many more of the lowest points in people’s lives can act as triggers for psoriasis, a skin condition that can produce agonizing, scaly skin across people’s entire bodies. For many patients, the experience is one of feeling at war with their own bodies, with the result that they have a sense of alienation from the self and from the world, from the physical and emotional touch of people and relationships.
After diagnosis, there comes for many patients, as well as the battle for treatment, a complete re-evaluation of themselves – their ambitions, their lifestyle, their relationships, their self-image. Many patients feel unable to live the life they want, finding it difficult to sustain a career and their social and romantic relationships. Mental health problems are common.
In the last decade, though, a new class of drugs – biologics – have become available. These have transformed the treatment of physical symptoms for many patients. For the first time, healthcare professionals have an option available to them that can, in many cases, rapidly and completely clear up a patient’s skin.
For patients, many who’ve experienced decades of suffering, a new treatment challenges their entire relationship with the condition. Clear skin alone is not enough – it leaves their need for emotional support unaddressed. They need not just medication, but to build a sense of self-belief and empowerment, so they are equipped to embrace their condition and its ups and downs. For healthcare professionals, many of whom have traditionally viewed psoriasis as an unfixable problem, these new treatments demand they rethink their entire practice.
Underpinning these challenges is the question of emotional, psychological and social support. How do dermatologists find the resources and expertise to help address patients’ psychological well-being, to help them embrace the potential of the treatment and face-up to the potential pitfalls? How does one help people with psoriasis embrace their condition and begin a new life full of possibilities? This is deep emotional territory. Unless one understands all the many facets of the condition and sees it in the round, how does one communicate with these patients? What does one say to them?
Addressing patients’ psychological and social wellbeing is a particular challenge for pharmaceutical companies because a traditional narrative in healthcare – protection – is beginning to lose its hold culturally. How does one frame the treatment for a world where people are no longer prepared to live in fear of their condition, its symptoms and its social and emotional impact? How does one support patients and help them remove their protective mask and show their real self to the world? How does one help them on a journey to self-acceptance and flourishing with their condition?
What is that narrative? This is the task this research set out to answer…
THE CLIENT CONTEXT
A major pharmaceutical company, referred to here as Pharma Living Well (PLW), wanted to better understand its customers: ‘moderate to severe psoriasis patients and health care professionals (HCPs) who prescribe or influence the prescribing of biologics’. Truth Consulting, a global strategic consultancy, specializing in innovation and branding, won the contract to understand the unmet needs of patients and HCPs in defining a digital strategy to support marketing communication and what solutions should be created. The Digital Work Stream – Goal Statement articulates the goal:
“To have a deep understanding of the informational needs of our target customers and be in a position to create findable, relevant and tailored digital content. It’s easy to go straight to solutions from what we think our customers would like, we would like to inform this process by “knowing what they want and expect from us” and by several means not just asking them, but observing what they do and co-creating solutions. What we learn will inform global solutions, regional solutions, affiliate solutions, medical education and utilisation of existing assets”. The Digital Work Stream – Goal Statement
Alongside its key PLW client contact, who had a regional role in the insights department, Truth Consulting soon realized that the underlying focus of this project was much bigger than a digital strategy. It was clear that this work had the potential to support new strategic foundations that PLW has adopted in its work in psoriasis – and possibly in other therapy areas too. The scope of the project grew beyond the original digital focus as shown in Table 1, with subsequent phases signed-off to explore in detail the emotional journey of people with psoriasis – and those that treat them. The Client Project Lead articulates this ambition:
“There was an opportunity to redefine expectations. We redefined our objective to create a bold ambition for the brand. Just as PASI75 (level of skin clearance) is not enough, information isn’t enough. There is a huge, unconquered territory for brands who see not just patients, but people and who can supply emotional support and understanding. If we see ourselves as enablers supporting people with psoriasis, people who take a holistic view of people’s lives, loves, ambitions and fears, then we can be the ones to fill that unmet need”. Client project lead
Table 1. The three phases of the project
| Phase 1 DISCOVER Foundational insights, strategic direction & solution ideation |
Phase 2 DEFINE Prototype development in co-creating and optimizing solutions & shaping final strategy |
Phase 3 DELIVER Development and rollout of the final solutions and strategic direction across markets |
|---|---|---|
| Aug 15 – Dec 15 | Jan 16 – July 16 | July 16 – Ongoing |
| Markets: Germany, UK & Canada |
Markets: Germany, UK, Canada & Spain |
Markets: Regional / global focus |
| Research • Cultural & social discourse analysis • In-home ethnographies • HCP depth-interviews • Co-creation online community with patients/HCPs • Co-creation workshop with patients/HCPs and clients |
Research • Prototype workshop and development • Key opinion leaders (KOLs) and patient influencer interviews • In-home ethnographies • HCP depth interviews • HCP & patient roundtable discussions • International workshop patients/HCPs/KOLs and clients |
Not a requirement for this stage by Truth – patients, HCPs, KOLs continue to be involved in development of solutions through advisory boards and workshops undertaken by client, development agencies and patient advocacy group partnerships |
| Internal engagement • Rich ethnographic storytelling • Series of workshops at key stages • Magazine style report |
Internal engagement • Rich ethnographic storytelling • Design thinking / prototyping to build to think • Behavioral economics heuristics framework for behavior change |
Internal engagement • Insight immersion workshops and toolkit • Briefing development agencies • Animation bringing to life the project |
| Output • Strategic plan and roadmap for the brand • 50+ solution ideas prioritized to take forward into phase 2 |
Output • 7-8 prototype solutions • Guidelines and manifesto for strategic delivery & solution development |
Output • Development of solutions (by appointed agencies) • Partnership with Global Patient Advocacy Group • Publication of key findings to impact standard of care |
Table 1: Having completed phase 1, Truth pitched and won phase 2 to take the insights and solution ideas from phase I into the creation of prototypes and final solutions. Phase 3 involves an ongoing consultancy role to support the delivery and immersion of the wider business and partner agencies in the insights and findings as the strategic direction and solutions are rolled out across markets. Note: a quantitative element to the project was undertaken in phase 2 by another agency to evaluate and validate the unmet needs of patients and HCPs.
PLW assembled a cross-functional team which included: Truth’s key client contact, insight team members in each of the key markets and representatives based across the region and from different parts of the business: medical, marketing/brand and digital. The core team played a key role in the success of the project, ensuring buy-in and engagement internally and, crucially, by helping navigate the many challenges the project faced. Some of these challenges included:
- Methodological questions – PLW, and pharmaceuticals generally, have established ways of working – ways of working that rarely accommodated elements of the proposed approach like in-home ethnographies, and cultural and social discourse analysis.
- Multiple markets – the project had to align the needs of numerous national markets regionally and then align those needs and outcomes with PLW’s global activities.
- Compliance – the project team had to work extensively with PLW’s legal team to achieve sign-off for elements of the research that would previously have considered to present unacceptable business risks – like bringing together HCPs and patients in the same forum.
TRY, TRY AGAIN
The recruitment process held many challenges, not least the long lead times needed to account for PLW’s internal processes and implement the relevant country-by-country legal and ethical pharma guidelines.
Truth worked with local market partner agencies in each of country, spending considerable time shaping the recruitment screeners and briefing the agencies to ensure all elements of the recruitment process were water tight. In each phase, a number of participants – patients, HCPs, thought leaders – were invited to take part in more than one element of the research, allowing them to come on the journey adding to the richness of the insight gathered.
Thought leaders played a key role in the project in adding their expertise as specialists and key opinion leaders. They included specialist dermatologists and nurses, psychodermatologists, patient influencers involved with patient advocacy groups – all recognized as leading in their field. With a set of criteria agreed with the PLW, Truth undertook desk research to identify the thought leaders and used snowballing sampling approach, drawing on thought leaders to recommend other thought leaders that they felt would be interested in taking part in the research.
There was a real sense of achievement across the Truth consulting team and the PLW core team when the teams met recruitment goals along the way. In particular, getting approvals was a challenge that often came right down to the wire. In places, the ‘try, try again’ attitude of the project team (Truth and client side) was called upon with creative solutions and certain compromises needed. For example, we intended to involve patients, healthcare professionals and thought leaders in the first co-creation workshop clients face-to-face. In the end, we had to hold virtual breakout sessions instead as part of the workshop. It was still judged a success. As a senior business leader articulates, it provided the first collective recognition of the key insight that clear skin alone isn’t enough:
“Understanding that clear skin and medication isn’t enough was foundational in the way we started to approach our role in supporting people with psoriasis. This key moment of realization came when listening to patients share their stories and how even when they achieve clear skin through their treatment that the fear of psoriasis and the impact of the emotional burden is always there for them.” Senior business leader
FROM INSIGHT TO POWERFUL REAL WORLD IMPACT
Our collaborative approach aimed to capture and share first-hand people’s stories. Truth Consulting was clear about what we would need to achieve the ambition of creating real world impact.
We wanted to enable storytelling and help everyone to directly experience the stories of others. We wanted to provide rich, balanced insight from immersion into conceptual spaces which people are not required to, or even able to, fully articulate. We wanted to look deeper to understand the connections that make us who we are. We wanted to help our client move beyond the corporate healthcare worldview and embrace the reality of patients’ lives.
Drug companies have treatments for psoriasis, but the emphasis is heavily on tackling physical symptoms. No one in pharma – PLW or beyond – was talking about what’s happening psychologically – and how that affects a patient’s relationship with his or her social world. A key realization, then – and one that underpinned the whole project – was that, “You can’t hope to understand psoriasis unless you look beyond the ‘patient’ – at the whole person.” To do this meant new depths of psychological and cultural insight. A transformative approach was needed to make sense of it all. One that explored the patient journey – physically and emotionally – and that looked to understand the daily realities of living with psoriasis.
Truth proposed a collaborative, immersive approach that would blend a wide range of techniques. The approach would explore broader cultural discourses around body image, bringing together doctors, patients and thought leaders (leading dermatologists and psychodermatologists, specialist nurses, advocacy group and patient influencers) and client representatives with the aim of helping all sides to learn from one another, to step into each other’s shoes and to commit to building a better future together. The multiple approaches used (see below) endorsed different ways of thinking to support patients with ground breaking services that address emotional suffering, and to change how patients and doctors perceive their roles. The mix of approaches that were blended together created productive tensions and alliances that allowed for collaborative sense-making conversations amongst the Truth project team and the client team. These included:
- In-home ethnographies to explore the realities of living with psoriasis – these took place in phases one and two, allowing not just insight gathering in the context of patients’ homes but also prototyping to take place in that same context, where the realities of living with psoriasis were most present.
- Cultural intelligence, like big data and semiotics, to smash ‘corporate world’ ‘unreal’ thinking. This highlighted social understanding and shifts in how culture framed skin/skin related diseases and wellness. How people talked about their condition in social spaces, i.e. the language, tone of voice, context, etc.
- Roundtable debate forums to reveal patient worlds hidden from clinical practice.
- A behavioral economics framework drawing out heuristics for behavior change.
- Quantitative evaluation and validation of unmet needs across patients and HCPs (undertaken by a different agency).
- Co-creation and design thinking approach in creating prototypes with designers, patients, doctors, and thought leaders to create useable, meaningful services.
In scope, this project was a huge undertaking. It covered four markets – Germany, Spain, Canada and UK. It incorporated 1000s of cultural conversations online; 72 hours of in-home ethnographies with patients; 54 hours of healthcare professionals (HCPs) interviews; 24 hours of thought leaders and patient influencers interviews; 24 hours of interactive debate between patients and dermatologists; and, a 2-week online co-creation community with 60 patients and 45 HCPs. Finally, it included 2 days of co-creation workshops with clients, patients, patient influencers, healthcare professionals and thought leaders.
The result has been an unprecedented depth of understanding into what it means to live with psoriasis, the barriers to seeking and receiving effective treatments, and how healthcare professionals and pharmaceutical companies can better support people with the condition. This project has generated a range of solutions designed with patients, to improve the support they receive; several published medical papers, and a piece in the Economist.
An industry-first partnership between PLW and the global patient association for people with psoriasis was a direct result of the project. This partnership, which shows a remarkable degree of pharma-patient group engagement, has been founded to ensure the research findings become embedded in the whole patient journey globally.
Finally, and perhaps most tellingly, the work has begun to change minds inside PLW, challenging established ways of working and redefining what best practice looks like. The global patient association partnership has been instrumental in effecting this change, with internal stakeholders appreciating the value of such human-centered insight and the real world impact the work can have.
THE APPROACH IN DETAIL: LAYERING OF INSIGHT
At each step of the journey, a recognition that communicating the richness of insight and the experiences and needs of people with psoriasis was going to be key to the success of this project guided the project team. The approach embedded the power of storytelling not only to gather insight but to bring to life the realities of living with psoriasis. Encouraging a narrative ‘storytelling’ approach allowed people to think freely and imaginatively, and enabled thinking at a higher level of narrative that tapped into fundamental emotional drivers and goals.
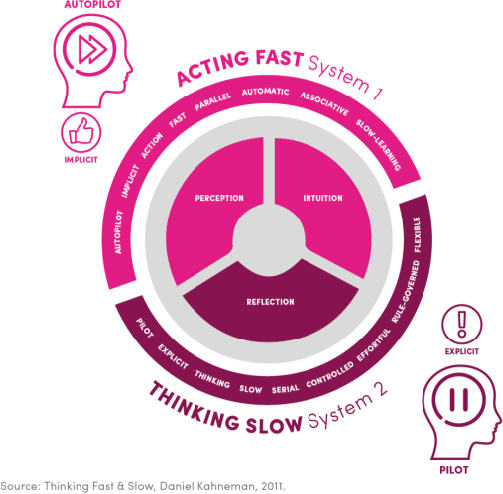
Nobel Prize-winning psychologist Daniel Kahneman produced a framework (Figure 1) showing the two systems that determine our decisions and behavior (Kahneman 2011). A useful metaphor for how the two systems work together is to see System 1 as an autopilot (implicit) and System 2 as a pilot (explicit). In this project, it was clear that deeper, implicit drivers were at play and that understanding the implicit goals of people with psoriasis and those that treat them was fundamental to creating a new and empowering narrative. Knowing that the ‘language’ of System 1 is built around associative and visual storytelling, key to achieving this new more positive narrative was to create stories and experiences that build associations and connections with people’s implicit goal.
Figure 1: Framework to help to make sense of the complexity of human behavior
This case study highlights the value of the ethnographic and other methodologies used in helping to create the internal engagement that can stimulate new and creative thinking in organizations and act as a catalyst for strategic level change across a business.
“Our findings show that ethnographic storytelling – the crafting of stories that takes place after an ethnographers’s immersion in the field – can be indispensable not only to a company’s consumer research function but also in changing the company’s strategic direction”. (Cayla, Beers and Arnould 2014)
The above quoted paper, Stories That Deliver Business Insights (2014), builds on this to outline “how ethnographic research can offer deeply emotional insights that increase organizational empathy”. But how does one achieve this ‘customer empathy’?
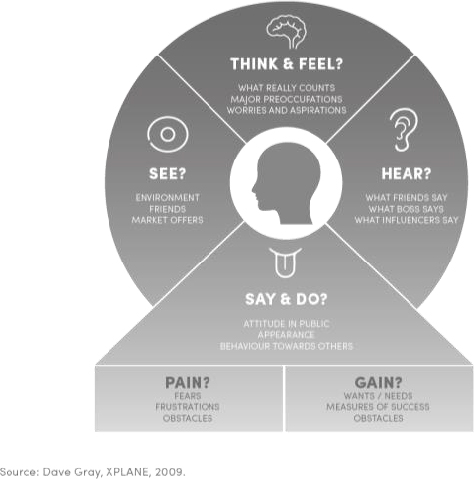
Figure 2: Empathy map used as a model to build empathy with customers
As shown in Figure 2, the combination of in-home ethnographies alongside methods such as cultural analysis allowed a layering of insights into spaces that people may struggle to articulate, or are unaware are influencing them directly e.g. wider cultural discourses on body image. Additionally, bringing patients, dermatologists, nurses, thought leaders & patient influencers together with clients – in roundtable debates and co-creation workshops – aided exploration of the tensions that existed between groups while allowing people to step into the shoes of others using the principles of design thinking and prototyping.
1. Cultural and Social Discourses
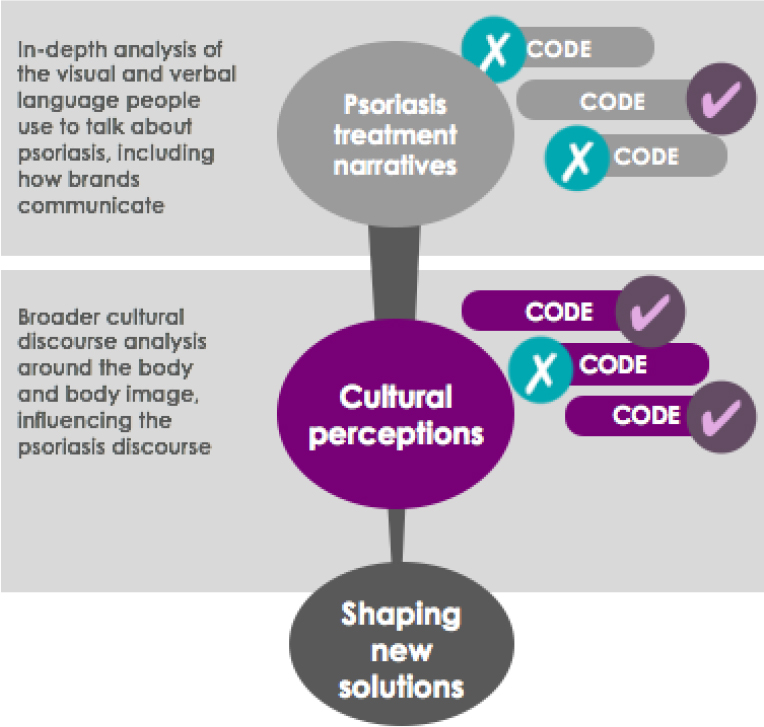
In order to better understand people, culture was the first port of call. This focus on culture provided rich, balanced insight from deep immersion into a conceptual space which people are not required to, or even able to, fully articulate. Looking at emergent discourses and ideas encoded into communications (Figure 3) provided the consulting team with an understanding of shifting needs of patients and a framework of understanding about what shapes the perceptions of patients, medical professionals and the general public. The team used an understanding of these influences to build empathy, connecting and providing strong relevance across all audiences.
Figure 3: The discourse analysis involved the critical examination of the cultural factors influencing perceptions and behaviors, using a semiotic lens to decode the verbal and visual language used.
Broader cultural discourses around body and body image were explored and an in-depth analysis undertaken of the visual and verbal codes including brands that people use to talk about psoriasis. The research was undertaken by a team of three semioticians, each responsible for their native market; Germany, Canada and UK. The following range of sources were explored:
- Academic publications and communities on body image, skin conditions etc.
- General cultural discourses on beauty, body and body image.
- Psoriasis-specific health, wellbeing and lifestyle discourses.
- Social media conversations on Twitter, Facebook, YouTube and other platforms.
- Traditional media, such as news and magazine coverage.
- Entertainment media, inc. film and TV representations of health & skincare topics.
- Pharmaceutical advertising, marketing and branding communications.
The analysis looked to unearth how other pharma companies communicate and uncover the underlying messages from the visual and verbal cues they use to get an accurate sense of how the different brands play into the psoriasis discourse. A second component of this analysis focused on culture, the team looked at how the visual and verbal language of the therapy area and related skin conditions are represented in conversation, TV, press, celebrity, books, etc. Culture is constantly changing and how we talk about skin conditions and psoriasis evolves depending on the development of new needs and lifestyles. For example, CariDee English, the 2006 winner of America’s Next Top Model has psoriasis and this has altered cultural perceptions of the condition. To understand how to create a relevant story for the brand therefore, we needed to identify these shifts and pull out the right cues to create interest, resonance and leadership.
Working together, the semioticians and the consultancy team, through collaborative narrative sense-making discussions, the team analysed the significant body of data that emerged. A rich cross-cultural framework of understanding evolved into a model that would underpin PLW’s overall strategic direction in its approach to psoriasis.
For reasons of client confidentiality, it is not possible to share this model. The model however was instrumental in sparking a new way of looking at the patient journey. It moved from the transactional to the emotional, taking a holistic view of the lives of people with psoriasis. It showed clearly, too, that there was an opportunity to shape a much more positive narrative.
Below, in brief, are three of the key stories that emerged and that became central insight areas in shaping the final strategy;
Toward a more positive narrative – As shown in Figure 4, a new and more positive discourse: ‘connection’ has increasingly replaced the traditional narrative of ‘protection’ in healthcare. Traditionally among people with psoriasis, failure to conform to popular beauty ideals resulted in feelings of defensiveness and shame. Now, though, they are progressively responding with a more positive and determined tone. Stepping out of the shadows by those that do not fit in has become widespread – they are seeking to show their real self to the world, to remove their protective mask, to challenge themselves and the world to turn avoidance into embrace. By embracing self-acceptance and self-expression, through engaging in productive discourses with both the inner and outer self, a positive upward cycle unfurls.
Figure 4: An emphasis on learning to love what you have and a new kind of body ideal, one rooted in a celebration of authenticity and difference, is taking hold in the wider cultural landscape.
Figure 5: The broader cultural movement toward self-acceptance and self-expression is rapidly gaining sway within the psoriasis community. A determined tone characterizes psoriasis bloggers, which fits naturally into the reconfiguring of the challenge as a productive stage in a broader upward-facing life narrative.
Within this general trend, differences by market were found to exist:
- In the UK, a new breed of psoriasis bloggers and patient influencers is sharing their stories and raising awareness.
- In Germany, strong communities of support are developing, providing a space for people to reconnect with life.
- In Canada, while celebrities are starting to speak out, the ‘protection’ narrative still retains considerable influence.
The power of vulnerability & self-acceptance – As suggested in Figure 5, we found the courage to be vulnerable lies at the heart of moving from protection to connection – removing the protective mask to show the ‘real self’. The worlds of people with psoriasis can open up as they become attuned to the relationship between inner world strength and positive outer world expression. Learning to open up and be vulnerable underlies the journey to self-acceptance which is fundamental to the ability to connect.
“I am married, and I am lucky. My husband is that rarest of creatures, the all-accepting, non-judgmental human being. It still took time for me to be comfortable for him to see me without my clothes, especially when my skin was flaring”. Female psoriasis sufferer, blog post
“After we started dating, it took a few months for us to finally get intimate and I knew something was bothering him, and he finally told me to much embarrassment that he had penile psoriasis. I was glad that he told me because I felt that he trusted me and, if anything, it made me love him more for his vulnerability and honesty”. Penile Psoriasis Halting Intimacy, blog post
It emerged that people with psoriasis typically go on a significant journey before coming to acceptance – a journey that can leave emotional scars. As a thought leader, specialist dermatologists and co-author of Global Report on Psoriasis, WHO (2016) outlined, “The emotional scarring can still serve as a burden to many patients – some hardly regain complete quality of life even though the skin is clear”. It was clear that there was a lot to be done in supporting people with psoriasis in achieving skin clearance and on their emotional journey to self-acceptance. This realisation acted as the impetus to extend the search for insights beyond understanding the patients’ journey and into inspiring solutions that could support, ease and shorten the journey toward self-acceptance and emotional well-being.
Turning toward to create an upward spiral of positive emotion – This brought the consulting team to the growing evidence that little touches are hugely important and that intimate relationships are full of bids for connection. These little touches and connections in our everyday lives are the secret behind many successful relationships.
Supporting people with psoriasis to build an upward spiral of positive emotion and turning towards connection in the micro-moments of everyday life, whether that be the courage to wear a short-sleeved top, or to reach out to a loved one, was integral to the overall strategic output of the project. As one expert said,
“A key coping strategy patients do is avoidance of activity. We want to help them to be more emotionally aware, access their feelings and expose their skin to other people. Even though patients have clear skin they still haven’t dealt with what’s underneath – our role is to facilitate a journey towards a renewed sense of self-belief and acceptance.” UK psychodermatologist – in-depth interview
One female patient provides an example of the value of this approach,
“By talking through the issues with a therapist it really helped me not to care so much. Afterwards, I bought my first short- sleeved top. I still remember the sense of liberation I got when I wore it for the first time. Putting my condition in perspective gave me a new sense of freedom. I realized that not everyone looking in my direction was staring at me.” UK female – online article
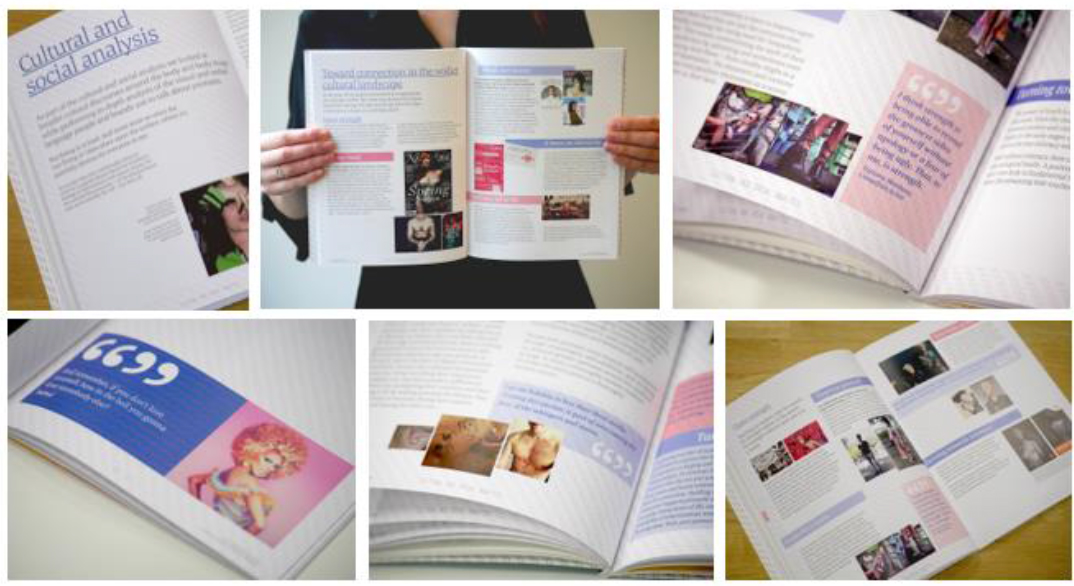
Figure 6: The richness of cultural insight and emergent discourses lent itself to powerful storytelling
In the first client workshop, the cultural analysis discoveries were shared with stakeholders from across PLW. The richness of cultural insight and emergent discourses stimulated a range of solution ideas which would be further developed based on the insights gathered in the in-home ethnographies and HCP in-depth interviews.
2. In-home Ethnographies & In-depth Interviews
Because of psoriasis’ deep psychological dynamics, the rich level of understanding we needed could only be gleaned in people’s homes. In-home ethnographies allowed the researchers to:
- Take cues from people’s homes, producing real stories whose deeper meaning emerged through sharing in context.
- Build a trusting relationship with people with psoriasis more rapidly by meeting them in a place of comfort and security.
- Use objects in the home as cues for detailed probing to explore unarticulated needs that wouldn’t naturally surface in a lab facility.
- Identify and explore differences between what people say they do and how they actually behave.
- Explore sensory experiences around their health and health experiences (Pink 2015).
It is hard to generalize about the impact of psoriasis except to say that the psychological impacts can be often worse than the physical ones and that, to understand a patient, you need to see their life in the round. The sometimes agonizing symptoms inevitably spill over into people’s emotional lives, drastically effecting their lifestyles, working lives and relationships. In situations like this, there is no substitute for hearing people tell their own story in their own words.
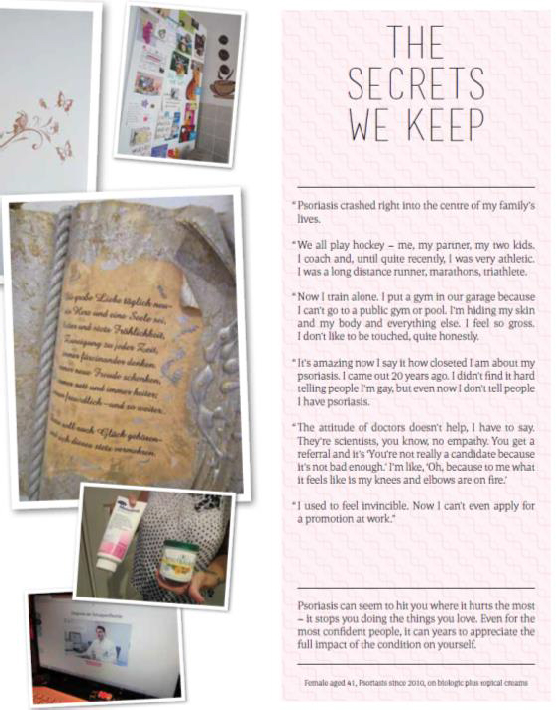
For example, one story from a hockey coach and triathlete whose physical prowess was a core part of her self-image, but found herself training at home, alone, too scared to go to the gym. “I used to feel invincible. Now I can’t even apply for a promotion at work.”
Figure 7: In-home patient stories in magazine style format to bring to life ethnographic storytelling as a tool to build empathy and engage internal stakeholders in the insights
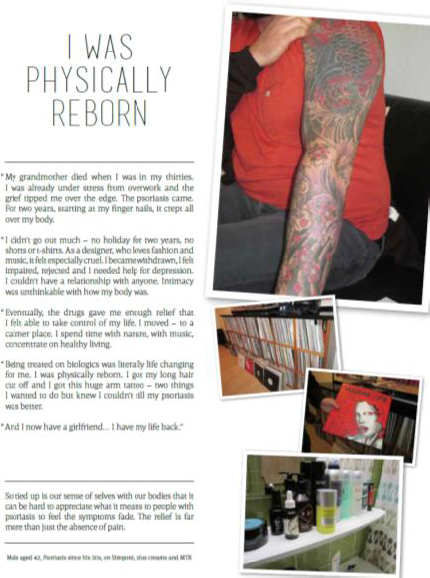
Another story comes from a man who, after growing more and more withdrawn, described the change on biologics as a ‘physical rebirth’. He cut off his long hair and, in an act of reclaiming his skin, got the arm tattoo he’d wanted for years. “And I now have a girlfriend…I have my life back.”
Figure 8: In-home patient stories in magazine style format to bring to life ethnographic storytelling as a tool to build empathy and engage internal stakeholders in the insights
Shared stories make it so clear that a good doctor-patient relationship is fundamental to recovery. As these verbatims show, patients can struggle to articulate the importance of the emotional aspect of psoriasis. HCPs widely overlook it:
“I would come with a list of questions and leave feeling ignored. Eventually, I saw I needed to take responsibility for getting well myself. I started to look for a doctor, dermatologist and rheumatologist who would work together. The big moment came when my dermatologist said to me ‘I believe you’. Just that. At last I had the possibility of being myself again.” Patient, Germany
“My dermatologist and I only ever discuss treatment – but sometimes I do want to say that I’m not feeling good… If my derm asked me how I was feeling I’d be more inclined to start to open up.” Patient, UK
As important as understanding patient perspectives was understanding the point of view of the medical professionals who treat them. The research therefore aimed to explore how dermatologists and patients could be empowered to have different and better conversations for a more effective management of patient treatment. As this dermatologist’s quote shows, it was clear there was much work to do, here: “I just don’t understand why it’s still having such a big psychological impact. You have clearance now, you need to let it go.” Thus, even where patients were on biologics, which was often a good indicator that patients and HCPs have entered a partnership approach to treatment, there were still gaps to be addressed.
It was clear that the patient-HCP dynamic needed to be rethought. Patients need to be empowered to overcome their fear of asking for more psychological help. HCPs, meanwhile, need better insight into the psychological impact of the condition. In these conditions, better-supported patients, better communication, and more effective and efficient consultations and treatment should result.
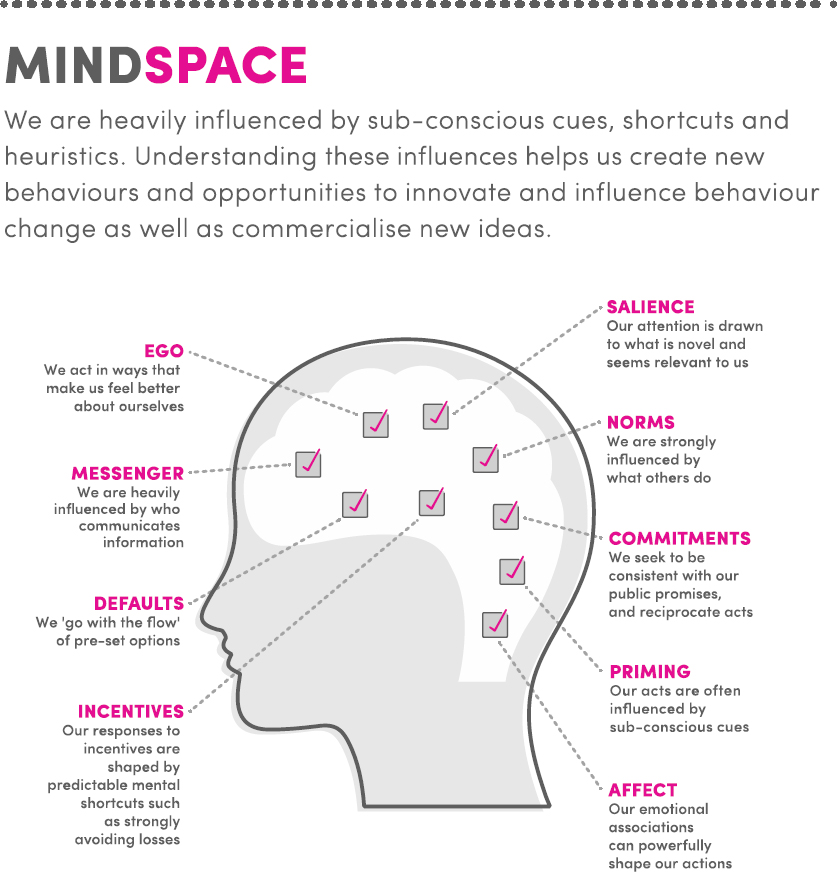
To understand the dynamics of the patient-HCP relationship and begin rethinking it, the MINDSPACE behavior change model was used. It was chosen as it outlines nine robust influences on human behavior and has been used successfully in shaping positive interventions in many areas of health, well-being and government policy.
Figure 9: Behavioural change framework MINDSPACE (2010) developed for policy makers, it looks at nine factors that influence and drive behaviour change. These factors are underpinned by considerable research from the fields of social psychology and behavioural economics.
The MINDSPACE framework, and the nine strands that comprise it, were used at multiple points in the project: in the development of discussions guides, as a framework for analysis (to identify which strands are most influential during the patient/HCP conversation) and to build behavior change interventions into the solutions created. Examples of some of the insights sorted by strand are as follows:
- INCENTIVES (our responses to incentives are shaped by predictable mental shortcuts, such as strongly avoiding losses) – Time a key barrier: “If you add only an extra 30-60 seconds to each patient that’s a whole extra hour a day and a hour that I am not getting paid for.” Dermatologist, Canada. A dermatologist may see more than 30 patients a day, usually for a maximum of 15 minutes. Practically, then, the opportunity to engage with psychological issues is limited, meaning patients can feel only the physical aspects of psoriasis are addressed.
- DEFAULT (We ‘go with the flow’ of pre-set options) – Focus on the visual: “Dermatology is a very visible discipline, you treat what you see in front of you and assess the rest by asking the right questions.” Dermatologist, UK. The treatment conversation remains dominated by physical appearance.
- PRIMING (Our acts are often primed by sub-conscious cues) – Inherent power inequality: Many patients recognize the lack of HCP interest in their wider lives and the belief their observations of their condition is given little weight in decision making. “I don’t even try now – they’re not interested in what I think or what I want to say.” Patient, Germany. As a result a gap can develop in the understanding of the impact of psoriasis on patients’ lives which affects the course of future treatment. Simply put, if HCPs don’t ask, patients won’t tell.
3. Co-creating a Better Future Together
Too often, research projects can stall in the transiting from insight to action. To ensure momentum could be generated and maintained, patients, dermatologists, nurses, thought leaders & patient influencers, alongside clients, were brought together to review the insights and ‘co-create a better future for people with psoriasis’.
A design thinking approach was taken to put empathy at the heart of the approach where all involved had the opportunity to step into each other’s shoes. From this viewpoint, a new understanding of the possibilities for change became real and a sense of commitment to sustained change was built (see final section Creating Strategic Momentum).
The building blocks of design thinking are:
- Empathy – insight grounded: this is about stepping into the patients and HCPs shoes and understanding the world from their perspective.
- Prototyping – build to think: prototypes are about making ideas, service concepts and experiences tangible. This allows ideas to be tested, refined with weaker ones discarded.
- Storytelling – bringing to life: this is about bringing to life and communicating insights and solutions in a way that moves people to action.
Truth’s consulting team included designers, illustrators and copywriters working together with the researchers, strategists and semioticians to guide the prototype development. A budget for the development of 7-8 concepts was allocated to include design, materials costs, and time involved.
The co-creation process involved the following immersive stages:
Co-creation auto-ethnographies – Over a two-week period through an online auto-ethnography and co-creation platform patients, dermatologists and nurses shared their experiences in shaping ideas & solutions that would better support the treatment of patients. Separate ‘streams’ for patients, dermatologist and nurses allowed each group to have their own ‘discussion space’. The timescale of the work allowed patients and HCPs to share their experiences of living with psoriasis (patients) and psoriasis treatment in general by completing 20 minute of auto-ethnography tasks daily – uploading pictures, videos and sharing stories with each other. This also zoomed in on their digital information search behaviours. Because it spread across multiple days, auto-ethnography supports an iterative approach, allowing co-creation/ideation over a longer period. Further, clients are able to ‘observe’ the community, enabling ongoing involvement in the research.
The research team moderated and stimulated the discussions by uploading tasks and sharing stimuli from the cultural analysis and in-home ethnographies. Shared in the form of insights linked to unmet needs, these stimuli were springboards for idea generation. Potential solutions from the previous phases were shared for each insight areas. For example, participants shared potential solutions to aid people in moving toward acceptance in an insight area exploring the power of vulnerability and self-acceptance. Through the co-creation process potential solutions were optimized and iterated and new ideas created.
At the end of the second week, a ‘focus group’ discussion allowed the participants to share their reflections on key emerging themes and which of the optimized solutions had the most potential in supporting their unmet needs.
Prototyping workshop – This was a working session with cross-functional & multi-disciplinary representatives from the client. The workshop aimed to immerse participants in key process insights and design thinking, and then agree which of the potential solutions would be taken forward into prototype development. As shown in Figure 10, as the participants brainstormed and shaped ideas, an illustrator was at hand to continuously draw the ideas to bring them to life.
Figure 10: The illustrations and sketches help inspire workshop participants in building out their ideas
A voting prioritisation process was used to select 7/8 ideas for the prototyping phase. The team went to work in bringing the prototypes to life – the ideas included a range of format such as apps, websites, paper based journal and storyboard animation (note: the prototypes cannot be shown in this paper for confidentiality reasons).
Involving influencers – With input from patient influencers and thought leaders, like leading dermatologists, specialist nurses, and psychodermatologists, prototypes evolved further. Input came from in-depth interviews across multiple markets, including hospital visits to understand the realities of treating patients in context and explore the potential to transform the standard of care.
“Our studies show that biologics without addressing the emotional needs will not have the impact on people’s overall sense of well-being. Training in the emotional area would be really good so dermatologists have a greater understanding of the psychological make up of patients – particularly on the one or two key questions that will help to understand where someone is emotionally on their journey”. Psychodermatologist thought leader
Roundtable debate forms – The research for this stage took place in moderated roundtable settings, allowing patients and healthcare professionals to properly listen to and understand each other. The 3.5hr sessions were held in a viewing facility with a large viewing room that allowed both HCPs and patients to observe each other exploring the prototypes before coming together to ‘debate’ and work together to provide optimal solutions. It was apparent, even in just a few hours, how much each had to learn from each other and how perspectives could change in a situation where honest, two-way communication could take place.
“Until I heard the patients explain how they suffered with psoriasis I had no idea that people were that deeply affected by the condition…I would definitely open up the conversation to the emotional now knowing this.” Dermatologist
As a result of this approach, we were able to extract not just deep insights, but powerful, personal expressions of what it means to live or work with psoriasis. It is clear that there is an opportunity to move toward a more equitable patient/HCP relationship by empowering patients to articulate their needs. HCPs, meanwhile, need better insight into the psychological impact of the condition that will support to meet patients’ holistic needs. Ultimately, putting more control in the hands of patients was seen as central to the solution development process – with solutions designed to support acceptance and a greater sense of control over themselves – both in terms of their emotional response and what they can achieve.
International co-creation workshop – Building on the previous phases, an international co-creation workshop with 3 Key Opinion Leaders, 3 dermatologists, 2 nurses and 6 patients and patient influencers set about prioritizing and optimizing the prototypes. Clients commented on the value of the co-creation workshops:
“This was EXCELLENT and should be the standard moving forward. Seeing derms and patients interact and learn about each other’s perspectives while they consult and actively engage in the creation of the final solutions was invaluable in creating meaningful solutions that have the potential to really make a difference”. Client stakeholder
“In my 25 years in pharma, I’ve never been involved in a situation where patients and HCPs have sat down together and told us what they need us to build for them and how they want it to work. Perhaps this is common in consumer markets, but in the world I work in, this is revolutionary.” PLW client
Having been on this journey together, the workshops transformed the tensions that were apparent in earlier stages of the project between the various groups of stakeholders. The co-creation workshops produced a positive spirit of togetherness.
Figure 11: Co-creation workshop with doctors, patients, thought leaders and the client teams
CREATING STRATEGIC MOMENTUM
The unprecedented depth of the project and the range of research methods employed, along with the feedback processes built in, give confidence that the outputs provide powerful insight into the world of psoriasis. Moreover, they give good reason to believe that it is possible to transform how psoriasis is treated and how people living with psoriasis, HCPs and the world generally think about the condition. In a sense, though, the bigger challenge – and one that faces any radical piece of research – is how to move from insight to impact. How to engender and sustain momentum over the period necessary to realize a bold vision is a challenge previous presentations at EPIC have emphasized (Hou & Holme 2015; Hoy & Rowley 2016). Hoy & Rowley (2016) argue that successful implementation is less a question of scale and more a question of whether the components of the network (the people and shared resources) have the capacity to deliver the strategy. These concerns helped shape the project approach. Owing to its size and regulated status, the pharmaceutical industry is inherently conservative. The risk was that the output of the project would face resistance from some quarters and undermine continuity in the support required for it to bear fruit. The client core team showed great courage internally in bringing colleagues, most notably compliance, on board. But the ‘network’ that was built went far beyond this. Patients, HCPs, patient influencers and, crucially, the global patient association partnership give the project many guardians who will provide the continuity and momentum necessary to ensure project outputs live on beyond the creative team.
To support the growth and effectiveness of this network, a host of initiatives are underway as part of the project’s delivery phase (Table 1):
- Immersion workshops – including toolkits and guidelines for roll-out.
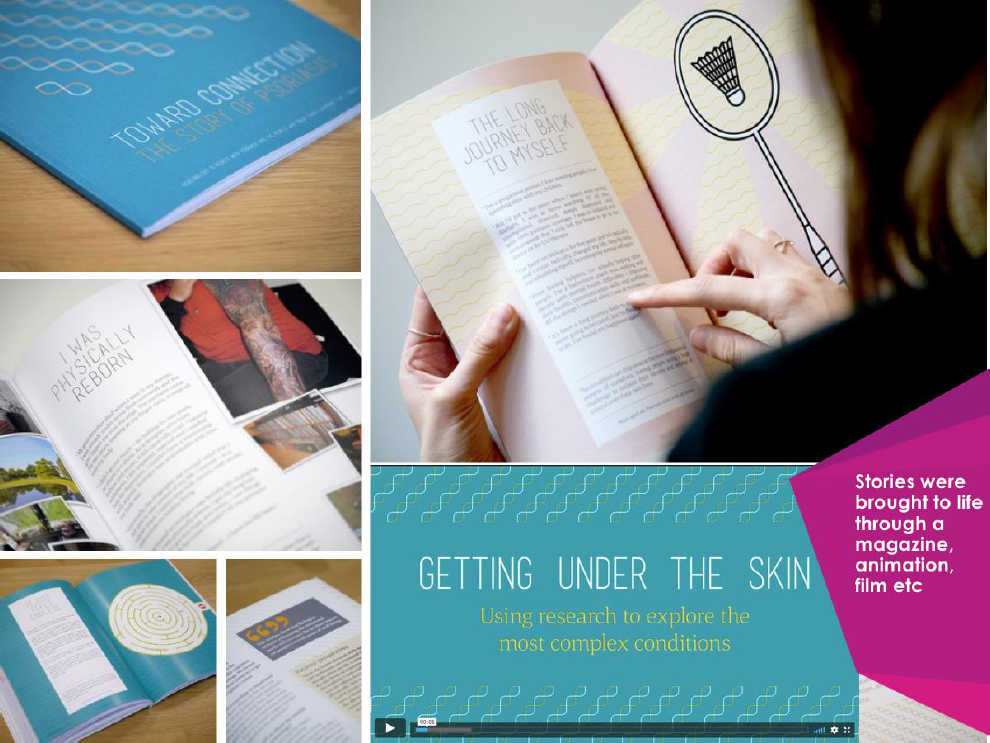
- Rich ethnographic storytelling – a magazine style report, an animation to bring to life the process, and foundational insight and manifesto posters.
- Solution development workshops – briefing agencies to begin to turn the prototypes into usable solutions.
- Best practice guidelines – sharing learnings on how to navigate and implement ethnographic and empathy driven methodologies.
- Publication of results in medical journals and The Economist – impacting professional discourse beyond the geographic confines of the project.
In all of this, the storytelling approach has proved crucial in overcoming objections and uniting the disparate groups involved in the project. It brought to life the realities of living with psoriasis as well as the perspectives of caregivers and HCP, fostering stakeholders’ emotional connections. In this sense, the power of story as a boundary object (Star & Griesemer 1989) moving across institutional borders allowed the various audiences to connect and take their meaning from the stories and embedded insights.
Figure 12: Stories were brought to life across the project to include a magazine, animations, film etc.
This has the potential to be a ground-breaking piece of work, providing deep, human-centered insight and, in so doing, helping to change how a global business thinks not just about its immediate customers, but about the very way in which it conducts its research.
Where once psoriasis was a devastating and hidden ailment, exacerbated by mutual misunderstanding between pharma, patients and HCPs, now the prospect is brighter in that research, through its network and strategic momentum, can support the transition to a new way of thinking about, and treating psoriasis. And do so for decades to come.
Sarah Kelleher is brand strategy director at Truth Consulting and specializes in bringing stories to life that engage, change behavior and solve challenging business problems. In her 20 years of working in the industry, Sarah has consulted on all aspects of branding, marketing, innovation and the power of contagious storytelling. sarah.kelleher@truth.ms
REFERENCES CITED
Cayla, Julien, Robin Beers and Eric Arnould
2014 Stories That Deliver Business Insights, Sloan MIT Management Review, VOL.55 NO.2.
Brown, Brené
2012 Daring Greatly How the Courage to Be Vulnerable Transforms the Way We Live, Love, Parent, and Lead. Gotham Books, Penguin Group. ISBN 13: 9781592408412.
Dolan, Paul, Michael Hallsworth, David Halpern, Dominic Kind and Ivo Vlaev
2010 MINDSPACE: Influencing Behaviour for Public Policy. Institute of Government, London, UK.
Hou, Carolyn and Mads Holme
2015 From Inspiring Change to Directing Change: How Ethnographic Praxis Can Move beyond. Ethnographic Praxis in Industry Conference Proceedings. https://www.epicpeople.org/from-inspiring-change-to-directing-change-how-ethnographic-praxis-can-move-beyond-research/
Hoy, Tom and Tom Rowley
2016 Strategy as an Unfolding Network of Associations. Ethnographic Praxis in Industry Conference Proceedings, p. 427–443, ISSN 1559-8918. https://www.epicpeople.org/strategy-unfolding-network-associations/
Kahneman, Daniel
2011 Thinking, Fast and Slow. Macmillan. ISBN 978-1-4299-6935-2.
Michalek, Irmina M, Belinda Loring and Swen Malte John
2016 Global Report on Psoriasis, World Health Organisation, WHO Library Cataloguing-in-Publication Data, ISBN 978 92 4 156518 9 (NLM classification: WR 205).
Papadopoulos, Linda
2005 Mirror, Mirror Paperback – Dr Linda’s Body Image Revolution. Acorn Digital Press. ISBN-13: 978-0340833766.
Pink, Sarah
2015 Doing Sensory Ethnography. Thousand Oaks, California: Sage Publications. ISBN: 978-1-4129-4803-6.
Star, Susan and James Griesemer
989 Institutional Ecology, ‘Translations’ and Boundary Objects: Amateurs and Professionals in Berkeley’s Museum of Vertebrate Zoology, 1907-39. Social Studies of Science. 19 (3): 387–420.